Imagine taking a pill for your anxiety, and within 30 minutes, you feel better. But by mid-afternoon, the effect fades, and you’re back to feeling overwhelmed. Now imagine another pill that takes hours to kick in-but lasts all day. Which one is right for you? The answer isn’t just about convenience. It’s about safety, effectiveness, and avoiding dangerous mistakes.
How These Two Types of Pills Work
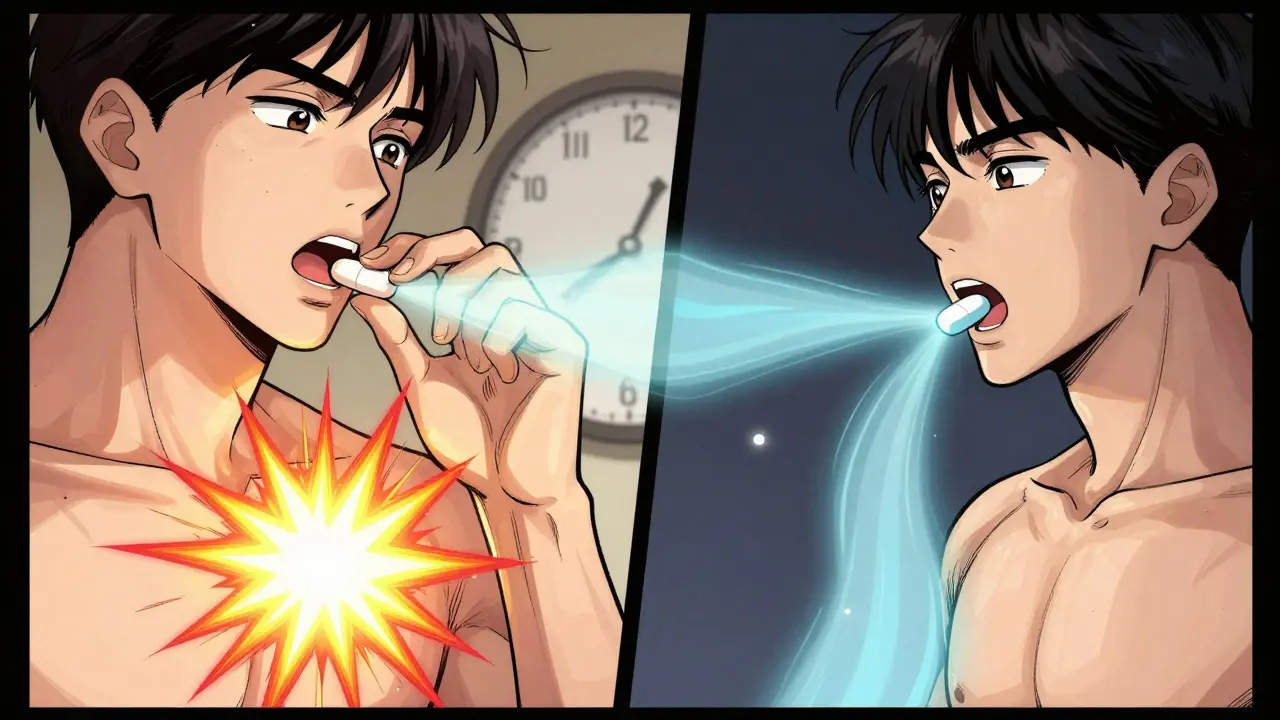
Immediate-release (IR) medications are designed to get into your system fast. As soon as you swallow them, the active ingredient starts dissolving in your stomach. Within 15 to 30 minutes, it’s in your bloodstream. Peak levels hit between 30 and 90 minutes. That’s why IR painkillers like ibuprofen or oxycodone work so quickly-they’re meant for sudden symptoms. Extended-release (ER), also called XR, SR, or CR, works differently. Instead of dumping all the drug at once, these pills release it slowly over 12 to 24 hours. Some use a gel-like coating that swells and leaks out drug gradually. Others have tiny beads inside that dissolve at different times. Some, like Concerta for ADHD, use an osmotic pump-basically a tiny water-powered pump that pushes the medicine out steadily. This slow release keeps drug levels steady. For example, bupropion IR can spike to 600 ng/mL in two hours, then crash below 100 ng/mL by the next dose. That rollercoaster causes side effects like jitteriness or insomnia. Bupropion XL, on the other hand, stays between 100-200 ng/mL all day. No spikes. No crashes. Just steady relief.Why Timing Changes Everything
Timing isn’t just about when you feel something. It’s about when the drug does its job-and when it might hurt you. Take Adderall. Adderall IR lasts 4-6 hours. Many kids with ADHD need a dose at school. That means a nurse has to administer it midday, which can be embarrassing and logistically messy. Adderall XR lasts 10-12 hours. One dose in the morning covers the whole day. A 2023 study at Laguna Treatment Center found that 89% of families preferred XR for this reason alone. But ER isn’t always better. If you’re having a panic attack, you don’t want to wait 2 hours for your medication to work. That’s why IR versions of benzodiazepines like lorazepam are still used in emergency rooms. The same goes for pain: if you’re in severe pain after surgery, waiting for an ER opioid to kick in isn’t an option. IR morphine or hydromorphone gives you relief now. The trade-off is clear: IR = fast action, short duration. ER = slow start, long-lasting effect.The Hidden Risks of Extended-Release
ER pills are safer for daily use-but riskier if something goes wrong. One of the biggest dangers? Crushing, chewing, or splitting them. Many ER tablets have special coatings or layers that control release. If you break them open, you’re basically turning a 12-hour pill into a 10-minute overdose. The FDA issued a warning in 2020 about this exact issue with extended-release opioids. People who crushed OxyContin tablets ended up with fatal blood levels of oxycodone. It’s not just opioids. A 2023 report from the Institute for Safe Medication Practices found that 23% of medication errors involving ER drugs happened because someone split a tablet that wasn’t scored. Venlafaxine XR, a common antidepressant, is a frequent culprit. Patients thought, “It’s just a pill-I’ll break it in half to save money.” Instead, they got a sudden rush of serotonin, leading to dizziness, rapid heartbeat, or worse. Another risk? Overdose recovery takes longer. If someone overdoses on IR bupropion, they’re usually out of danger within 8-12 hours. But with ER bupropion, the drug keeps releasing for 24-48 hours. Hospital stays are 2-3 times longer. The National Poison Data System recorded 41% more ER overdose complications in 2021 compared to IR.
When ER Wins (and When IR Is Better)
Not all conditions are the same. Here’s how doctors decide:- Chronic conditions (hypertension, depression, ADHD, diabetes): ER is usually preferred. A 2022 JAMA study of 15,000 hypertension patients showed 78% of ER users took their meds correctly over 12 months. Only 56% of IR users did. Fewer doses = fewer missed pills.
- Acute or fluctuating symptoms (pain, anxiety attacks, breakthrough symptoms): IR gives you control. A Reddit user with ADHD wrote, “I take XR for work, but keep 5mg IR tabs for presentations. If I need instant focus, I don’t wait.”
- Titration phases (when you’re adjusting your dose): IR is essential. If you’re starting a new antidepressant, your doctor will likely begin with IR so they can fine-tune the dose quickly. Switching to ER too soon can mask side effects or delay finding the right level.
- Patients with digestive issues: ER can be unpredictable. The FDA warned in July 2023 that people with gastroparesis (delayed stomach emptying) absorb ER meds too slowly-or too fast-leading to dangerous spikes. In these cases, IR may be safer.
Cost, Adherence, and Real-Life Trade-Offs
ER pills cost more. Adderall XR runs $350-$450 for 30 capsules. Adderall IR is $280-$380. That’s a 15-25% premium. But here’s the catch: higher cost doesn’t always mean worse value. A 2022 GoodRx survey of 5,000 chronic medication users found that 41% didn’t understand how ER worked. Many thought, “If I don’t feel anything after an hour, I must need another pill.” That led to 9% unintentionally overdosing. Patient education is critical. On the flip side, adherence improves. For people taking meds for depression, anxiety, or high blood pressure, taking one pill a day instead of three or four makes a huge difference. The CDC reports that 68% of new antidepressant prescriptions in 2022 were ER versions-not because they’re stronger, but because people stick with them. And yes, some patients notice the difference. Metoprolol ER users reported 32% fewer dizziness episodes than those on IR. But 27% of them complained the medication didn’t help fast enough during panic attacks. That’s not a flaw-it’s a design choice.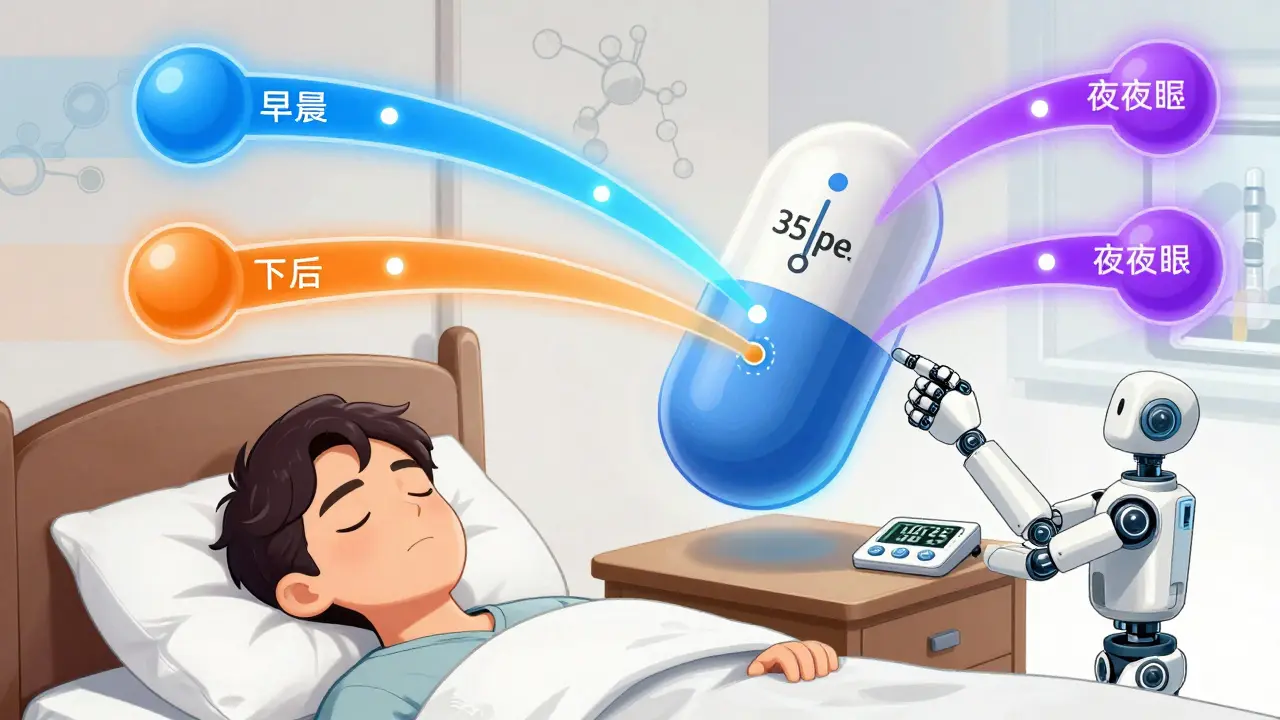
What You Need to Know Before You Take Either
If you’re prescribed an ER medication:- Don’t crush, split, or chew it. Ever. Even if it looks like a regular pill.
- Wait at least 2-4 hours before deciding it’s not working. It’s not supposed to kick in like IR.
- Don’t double up if you miss a dose. Take it as soon as you remember, but skip it if it’s almost time for the next one.
- Check the label. If it says “do not open capsule” or “swallow whole,” that’s not a suggestion-it’s a safety rule.
- Set alarms. Missing a dose means your drug level drops fast.
- Carry a backup if you’re traveling. Running out means symptoms can return suddenly.
- Don’t assume IR is “weaker.” It’s just faster and shorter-lived.
What’s Next for Medication Timing?
The future of drug delivery is getting smarter. Researchers at MIT are testing 3D-printed “polypills” that release different drugs at precise times-like one for morning blood pressure, another for afternoon pain, and a third for nighttime sleep. These aren’t available yet, but they show where the field is headed. Meanwhile, companies like Impax Labs are building abuse-deterrent ER formulas. Their Aversion® technology turns crushed pills into a thick gel, making them hard to snort or inject. Early data shows a 47% drop in abuse rates for ADHD meds using this tech. But for now, the choice between ER and IR remains simple: it’s not about which is better. It’s about which is right for you-and your body’s timing.Can I split an extended-release pill if it’s too expensive?
No. Most extended-release pills are not designed to be split. Splitting them can destroy the slow-release mechanism, causing a dangerous surge of medication all at once. Even if the pill looks like it has a score line, it may not be safe to break. Always check the label or ask your pharmacist before splitting any medication.
Why does my ER medication take so long to work?
Extended-release pills are built to release medication slowly over 12-24 hours. It can take 2-4 hours just to reach therapeutic levels. This is normal. If you feel no effect after an hour, don’t take another dose. You’re not being slow-you’re just following the design. Waiting too long to feel results is why many people accidentally overdose.
Is extended-release always better than immediate-release?
No. ER is better for long-term, stable conditions like high blood pressure or depression, where steady levels reduce side effects and improve adherence. But for sudden symptoms-like a panic attack, acute pain, or a breakthrough seizure-IR is faster and more effective. The best choice depends on your condition, lifestyle, and how your body responds.
What happens if I accidentally crush an ER pill?
You may get a sudden, potentially dangerous dose of medication. For example, crushing an ER opioid can cause respiratory depression or overdose. Crushing ER bupropion can trigger seizures. If this happens, call Poison Control immediately (1-800-222-1222 in the U.S.) and seek medical help. Do not wait for symptoms to appear.
Can I switch from IR to ER or vice versa on my own?
Never switch without talking to your doctor. ER and IR versions are not interchangeable. A 20mg ER tablet does not equal a 20mg IR tablet in how it affects your body. Switching without guidance can lead to underdosing, overdosing, or dangerous side effects. Always follow your prescriber’s instructions.
If you’re unsure whether your medication is ER or IR, check the label. Look for XR, ER, SR, CR, or XL after the drug name. If you’re still not sure, ask your pharmacist. It’s one question that could prevent a hospital visit.
So let me get this straight-you’re telling me I can’t crush my Adderall XR to get a quick high but I can just swallow a bunch of IR tabs and call it a day? Classic. The system is rigged. I mean, if the drug companies wanted us to be safe, they’d make the pills taste like candy and come with a free therapist. But nooo, they want us to suffer through 2-hour delays and then pay $400 for the privilege. This isn’t medicine, it’s a luxury subscription.
And don’t even get me started on the ‘don’t split the pill’ nonsense. I’ve split aspirin since I was 16. What’s the worst that could happen? I die? Maybe. But at least I died trying to save $20. RIP me in 2025.