When your body turns against itself, everyday tasks become mountains. Getting out of bed, tying your shoes, holding a coffee cup - these aren’t just chores. For people with autoimmune diseases like lupus, rheumatoid arthritis, or Sjögren’s syndrome, they’re battles. And the fatigue? It’s not just being tired. It’s a deep, bone-heavy exhaustion that no amount of sleep fixes. This is functional impairment - when your disease steals your ability to do the things you need and want to do. But here’s the truth: rehabilitation isn’t about fixing your disease. It’s about reclaiming your life despite it.
Why Functional Impairment Happens in Autoimmune Diseases
Autoimmune diseases don’t just cause joint pain or rashes. They trigger chronic inflammation that damages tissues, nerves, and muscles over time. Medications help, but they come with side effects - muscle weakness, balance issues, or even more fatigue. Then there’s the silent thief: deconditioning. When you stop moving because every step hurts, your muscles shrink, your stamina drops, and your body forgets how to do simple things. A 2022 study in the Journal of Autoimmunity found that without intervention, functional decline can accelerate by up to 42% in the first year after symptoms begin. That’s not just bad days. That’s losing your independence.Physical Therapy: Rebuilding Strength Without Ignoring Flares
Physical therapy (PT) isn’t about pushing through pain. It’s about moving smart. During a flare, when joints are swollen and hot, therapists start with gentle isometric exercises - muscle contractions without joint movement - at just 20-30% of your max effort. That’s not a joke. It’s science. Pushing too hard during a flare can make things worse, not better. A 2020 PMC review showed that even light, controlled movement helps reduce stiffness without triggering a crash. As inflammation settles, therapy shifts. Aerobic training kicks in - walking, cycling, or swimming at 40-60% of your heart rate reserve. That’s not sprinting. That’s a pace where you can still talk but not sing. Underwater treadmills at 92-96°F are gold standard for many clinics. The warm water reduces joint pressure and eases pain, helping patients move more freely. One study found hydrotherapy cut pain scores by 22% compared to land-based exercise. But here’s the catch: 68% of rural clinics don’t even have access to these pools. That’s why home-based programs are becoming essential.Occupational Therapy: Making Daily Life Possible Again
If PT rebuilds your body, OT rebuilds your life. Occupational therapists don’t care how far you can walk. They care if you can open a jar, button your shirt, or cook a meal without collapsing afterward. Their secret weapon? The 4 Ps: Prioritize, Plan, Pace, Position. - Prioritize: What tasks matter most? Maybe it’s feeding your kids, not vacuuming. Focus there. - Plan: Break big tasks into small steps. Wash dishes one sink at a time, not the whole stack. - Pace: Work for 15-20 minutes, then rest 5-10. No exceptions. This isn’t laziness - it’s strategy. - Position: Use your body smart. Sit while brushing your teeth. Use a long-handled grabber to pick things up. A $15 tool can save you hours of pain. The Canadian Occupational Performance Measure (COPM) is the gold standard for tracking progress. A 2-point increase on its 10-point scale? That’s a real win. For one patient, it meant going from needing help to dress to doing it alone - and finally returning to part-time work.PT vs OT: What Each One Does Best
They work together, but they have different superpowers. - PT wins for lower body strength. If you struggle to stand from a chair or walk up stairs, PT improves your Timed Up and Go score by 28% more than OT alone. - OT wins for hands and daily tasks. If you can’t grip a toothbrush or open a pill bottle, OT improves your hand function by 33% more than PT alone. Think of it like this: PT gets you to the kitchen. OT helps you make the coffee.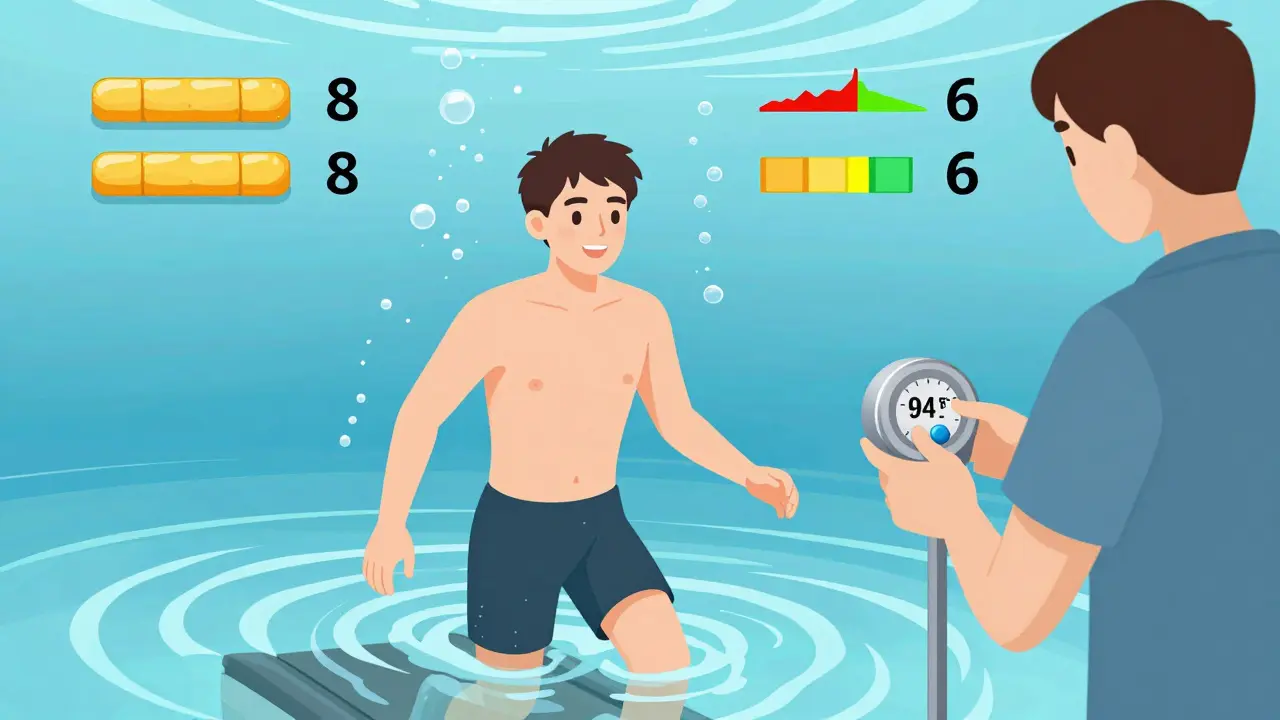
The 70% Rule: Why Pushing Too Hard Backfires
The biggest mistake patients make? Doing too much on good days. It’s called the boom-bust cycle. You feel okay - you clean the house, go shopping, take the kids to school. Then, for the next three days, you’re stuck in bed. Sixty-three percent of people with autoimmune diseases do this. It’s not willpower. It’s biology. The solution? The 70% rule. Never push yourself past 70% of what you think you can do. If you feel like you can lift 10 pounds, lift 7. If you think you can walk for 30 minutes, walk for 20. Use a heart rate monitor. If your heart rate spikes too fast, you’re overdoing it. Real-time feedback stops crashes before they start.Tools That Actually Work
You don’t need fancy gadgets. But some tools change everything: - Voice-activated smart home systems (Alexa, Google Home) let you turn on lights, play music, or lock doors without lifting a finger. One study showed a 31% increase in independence for people with hand impairments. - TENS units deliver gentle electrical pulses that block pain signals. Used at 50-100Hz, they’re safe and effective during flares. - Activity diaries - simple paper logs - help track what triggers fatigue. Over time, patterns emerge. Maybe you crash after standing for 12 minutes. Now you know to sit.When Therapy Doesn’t Work - And Why
Not every rehab program helps. And sometimes, it makes things worse. Why? - Therapists who don’t understand autoimmune disease push patients to “just keep going.” That’s dangerous. One Reddit user wrote: “My therapist made me run on a treadmill during a flare. I was bedridden for two weeks.” That’s not rehab. That’s harm. - Insurance won’t cover enough sessions. Most plans pay for 12-15 visits a year. Experts say you need 24-30 to see lasting change. That’s why home-based telehealth programs have exploded since 2020. Sixty-eight percent of patients now use them. - Central fatigue - the brain fog and exhaustion that doesn’t improve with rest - is often ignored. Dr. Alan Peterson warned in JAMA Internal Medicine that 19% of rehab programs don’t even measure it. If you have lupus or Sjögren’s, that’s a dealbreaker.
What to Look for in a Therapist
Not all PTs and OTs know how to work with autoimmune diseases. Look for: - Certification from the Academy of Pelvic Health Physical Therapy’s Autoimmune Specialty Program (120 hours of training, $1,200 fee). - Experience with at least 10 different autoimmune conditions. There are 87 recognized ones - your therapist should know the difference between lupus fatigue and MS fatigue. - Willingness to adjust based on your symptoms. If you’re having a flare, they should scale back - not push harder.The Future: Smarter, Personalized Rehab
The field is changing fast. In 2024, new guidelines will use blood markers like IL-6 to adjust exercise intensity. If your inflammation is high, you get a lighter workout. If it’s low, you can push a bit more. Early trials show 39% better outcomes. Apps like Lupus Foundation’s “PacePartner” are in final testing. They use wearable sensors to predict flares 48 hours in advance with 82% accuracy. Imagine getting a notification: “Your body is signaling a flare tomorrow. Reduce activity today.” That’s not sci-fi. It’s coming.What You Can Do Today
You don’t need to wait for perfect care. Start now:- Track your energy. Note what you do and how you feel afterward.
- Use the 70% rule - always.
- Break tasks into 15-minute chunks with rest in between.
- Ask your doctor for a referral to an occupational therapist - even if you think you’re fine.
- If your therapist pushes you through pain, find a new one.
Can exercise make autoimmune symptoms worse?
Yes - if it’s too intense or done during a flare. High-impact activities like running or heavy lifting can trigger flares in 23% of patients. But gentle, paced exercise improves function by 35-42%. The key is matching intensity to your current disease activity. Always stop if you feel a crash coming.
How long does it take to see results from rehab?
Most people notice small improvements in 4-6 weeks - better sleep, less stiffness, more energy. But meaningful changes in daily function - like being able to cook or dress yourself - usually take 3-6 months. Consistency matters more than intensity. Skipping sessions during flares is normal; returning to therapy when you’re stable is what builds long-term gains.
Is hydrotherapy better than land-based therapy?
During active flares, yes. Warm water reduces joint pressure and pain, helping you move more easily. Studies show 22% greater pain relief compared to land exercise. But if you don’t have access to a pool, land-based therapy with proper pacing still works. The goal is movement, not the location.
Can occupational therapy help with brain fog and fatigue?
Yes - indirectly. OT doesn’t treat brain fog directly, but it helps you manage it. By teaching energy conservation, simplifying tasks, and using tools like voice assistants, OT reduces the mental load. That leaves more energy for thinking. Patients report clearer focus after learning to pace themselves and avoid decision fatigue.
Why do insurance companies limit rehab sessions?
Because many insurers still treat autoimmune diseases like temporary injuries, not chronic conditions. Most plans cap therapy at 12-15 sessions per year, even though experts recommend 24-30. Some states don’t even have billing codes for autoimmune rehab, leading to 22% claim denials. Advocacy and documentation from your therapist can help - but it’s an ongoing battle.
What’s the most common mistake people make in rehab?
Doing too much on good days. This is called the boom-bust cycle. You feel okay, so you overdo it - cleaning, shopping, exercising. Then you crash for days. It’s the #1 reason people quit rehab. The solution? Stick to the 70% rule every day, no matter how you feel.

Man, this hit home. In India, we don’t talk much about autoimmune stuff - it’s all ‘just rest more’ or ‘eat turmeric.’ But this? This is real. I’ve got RA and my PT actually gets it. No pushing through pain. Just smart moves. Thank you for writing this.