When you’re breastfeeding, every pill you take feels like a risk. You wonder: will this medicine hurt my baby? The truth is, most medications do get into breast milk-but that doesn’t mean they’re dangerous. In fact, 98% of the drugs moms take while nursing are safe or pose minimal risk. The real issue isn’t whether drugs get into milk-it’s understanding how they get there, how much reaches your baby, and what actually matters for their health.
How Medications Get Into Breast Milk
Medications don’t travel to breast milk like a direct pipeline. They move through your body like everything else: into your bloodstream, then across the tiny walls of the milk-producing cells in your breasts. Most of this happens through passive diffusion. That means the drug follows the natural flow-from higher concentration in your blood to lower concentration in the milk. About 75% of all medications enter this way. The rest move through special transport systems. Some drugs, like nitrofurantoin or acyclovir, use protein carriers built into the milk cells. These systems are picky-they only move certain molecules. That’s why some drugs barely show up in milk, even if they’re strong in your blood. A few key factors decide how much ends up in your milk:- Molecular size: Drugs under 300 daltons (like lithium or sertraline) slip through easily. Anything over 800 daltons-like heparin-stays mostly in your blood.
- Lipid solubility: Fatty drugs (like diazepam) dissolve better in milk fat and transfer more. Water-soluble drugs (like gentamicin) barely make the jump.
- Protein binding: If a drug sticks tightly to proteins in your blood (like warfarin), it can’t leave. The more bound, the less goes into milk.
- Acidity (pKa): Your milk is slightly less acidic than your blood. Weak bases (like amitriptyline) get trapped in milk and can reach 2-5 times higher levels than in your blood.
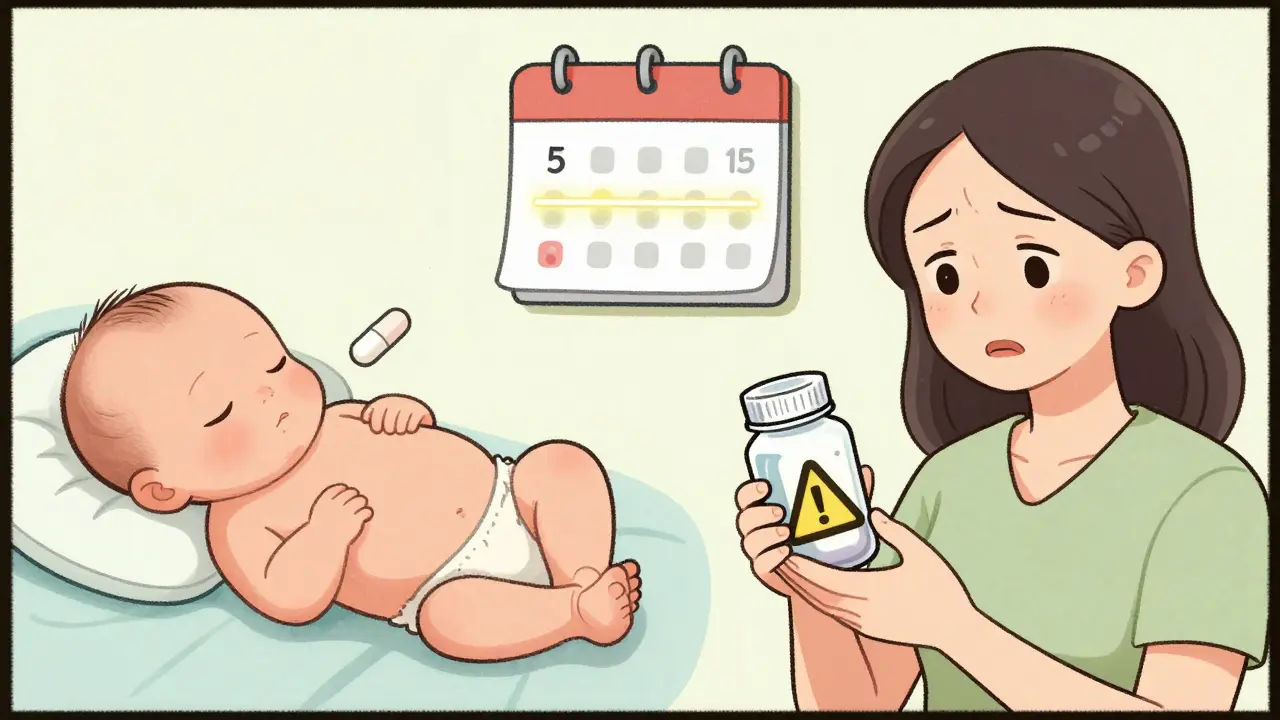
And here’s something most moms don’t know: right after birth, your milk ducts aren’t fully sealed. Between days 4 and 10, gaps between cells are wider-up to 20 nanometers. That means more drugs, even larger ones, can slip through. After day 10, those gaps close. That’s why timing matters. A drug you take on day 5 might affect your baby more than the same dose on day 15.
How Much of the Drug Actually Reaches Your Baby?
Just because a drug gets into milk doesn’t mean your baby gets a full dose. Most babies absorb only a small fraction of what’s in the milk-and even less enters their bloodstream. The general rule: if your baby gets less than 10% of your weight-adjusted dose, it’s usually safe. Most medications land far below that. For example:- Amoxicillin: Baby gets about 1.5% of your dose.
- Gentamicin: Less than 0.1% reaches the baby.
- Diazepam: Up to 7.3%-higher, but still low enough that most babies show no effect.
- Sertraline (Zoloft): 1-2% of your dose. The most common antidepressant used while breastfeeding.
But some drugs build up. If your baby is newborn, their liver and kidneys are still learning how to process things. A drug like phenobarbital can accumulate over days, reaching 15% of your dose by week one. That’s why doctors watch for signs like excessive sleepiness, poor feeding, or irritability-especially with long-acting drugs.
What Makes a Drug Safe or Risky?
Experts don’t just guess. They rate drugs based on decades of data. The most trusted system comes from the InfantRisk Center, founded by Dr. Thomas Hale. They rate drugs from 1 to 5:- Level 1: No detectable transfer. Examples: insulin, heparin, most antacids.
- Level 2: Minimal transfer, no reported harm. Examples: sertraline, amoxicillin, ibuprofen.
- Level 3: Limited data, possible risk. Use with caution. Examples: fluoxetine, some thyroid meds.
- Level 4: Possible risk. Avoid unless benefit outweighs risk. Examples: lithium, cyclosporine.
- Level 5: Proven danger. Avoid completely. Examples: radioactive iodine, chemotherapy drugs.
Here’s the big takeaway: 87% of commonly used medications are Level 1 or 2. That means you can likely keep breastfeeding while taking your prescription.
But not all sources agree. The European Medicines Agency warns about serotonin syndrome with SSRIs, citing rare cases of fussiness or poor feeding. The InfantRisk Center says those cases are extremely rare and often linked to high doses or other factors. This is why you need personalized advice-not just a list.
When Timing Matters
Taking your pill at the right time can cut your baby’s exposure by half. The best strategy: take your medication right after you breastfeed. That gives your body time to break down and clear the drug before the next feeding. For drugs with a 4-hour half-life, waiting 3-4 hours drops infant exposure by 30-50%. For long-acting drugs like diazepam (which can last 30-100 hours in newborns), timing isn’t enough. You might need to space doses or switch to a safer alternative. If you’re on a daily dose over 10 mg, your doctor might suggest checking your baby’s blood levels to be safe.Drugs That Can Hurt Milk Supply
Not all risks are about the baby. Some drugs hurt your milk production.- High-dose estrogen birth control: Pills with more than 50 mcg ethinyl estradiol can slash milk supply by 40-60% in just 72 hours.
- Bromocriptine: Used to stop lactation. It works-95% of women stop making milk within 5 days.
- Pseudoephedrine: A common decongestant. Even one dose can reduce milk output by 24% in some women.
If you’re trying to maintain supply, avoid these unless there’s no alternative. Talk to your doctor about safer options-like progestin-only birth control or saline sprays instead of decongestants.
What to Watch For in Your Baby
Most babies show no reaction. But if you notice any of these, call your pediatrician:- Excessive sleepiness or difficulty waking to feed
- Poor feeding or refusing the breast
- Unusual fussiness, crying, or irritability
- Rash or diarrhea (rare, but possible with antibiotics)
These signs are uncommon. In fact, studies show only 8.7% of babies on SSRIs show mild irritability, and only 5.3% have feeding issues. Most of these resolve on their own or with a small dose adjustment.
What’s New in 2026
The rules keep getting better. Since 2023, the FDA requires all new drugs to include breastfeeding data on their labels. That means more accurate info for moms and doctors. The InfantRisk Center’s LactMed app (version 3.2) now uses AI to predict risk based on 12 factors: your dose, your baby’s age, the drug’s half-life, your metabolism, and more. It’s not perfect-but it’s the most advanced tool out there. And research is moving fast. The NIH-funded MOMS study, running through 2025, is setting clear safety thresholds for 50 priority medications. That means in the next few years, we’ll know exactly how much is safe-not just “probably okay.”The Bottom Line
You don’t have to choose between your health and your baby’s. Most medications are safe to take while breastfeeding. The risk isn’t in the drug-it’s in the fear.Here’s what you should do:
- Don’t stop breastfeeding because you’re on a new medication-unless your doctor says so.
- Ask your doctor or pharmacist: “Is this safe while breastfeeding?” Don’t assume it’s not.
- Use the InfantRisk Center’s website or app to check your drug.
- Take meds right after feeding to minimize exposure.
- Watch your baby for signs of reaction-but don’t panic over small changes.
- If you’re on antidepressants, anticonvulsants, or thyroid meds, ask about monitoring your baby’s levels.
Over 80% of U.S. moms start breastfeeding. Nearly half quit early-not because of health issues, but because they were told to stop taking their meds. That’s a mistake. With the right info, you can keep nursing, stay healthy, and give your baby the best start.

Let me just say this: if you're taking anything stronger than ibuprofen and still breastfeeding, you're playing Russian roulette with your baby's neurodevelopment. The data is skewed by pharma-funded studies. That '98% safe' claim? Total nonsense. I've seen infants with liver enzyme spikes from sertraline exposure. Stop normalizing this.