Hypoglycemia Treatment Calculator
How to Treat Low Blood Sugar
When your blood sugar drops below 70 mg/dL (3.9 mmol/L), you need fast-acting glucose to raise it safely. Follow these steps:
- Use 15g of fast-acting glucose for blood sugar below 70 mg/dL
- Wait 15 minutes and recheck your blood sugar
- Repeat treatment if necessary
- After your sugar rises, eat a small snack with protein or complex carbs
Enter your blood sugar level to calculate the correct treatment amount.
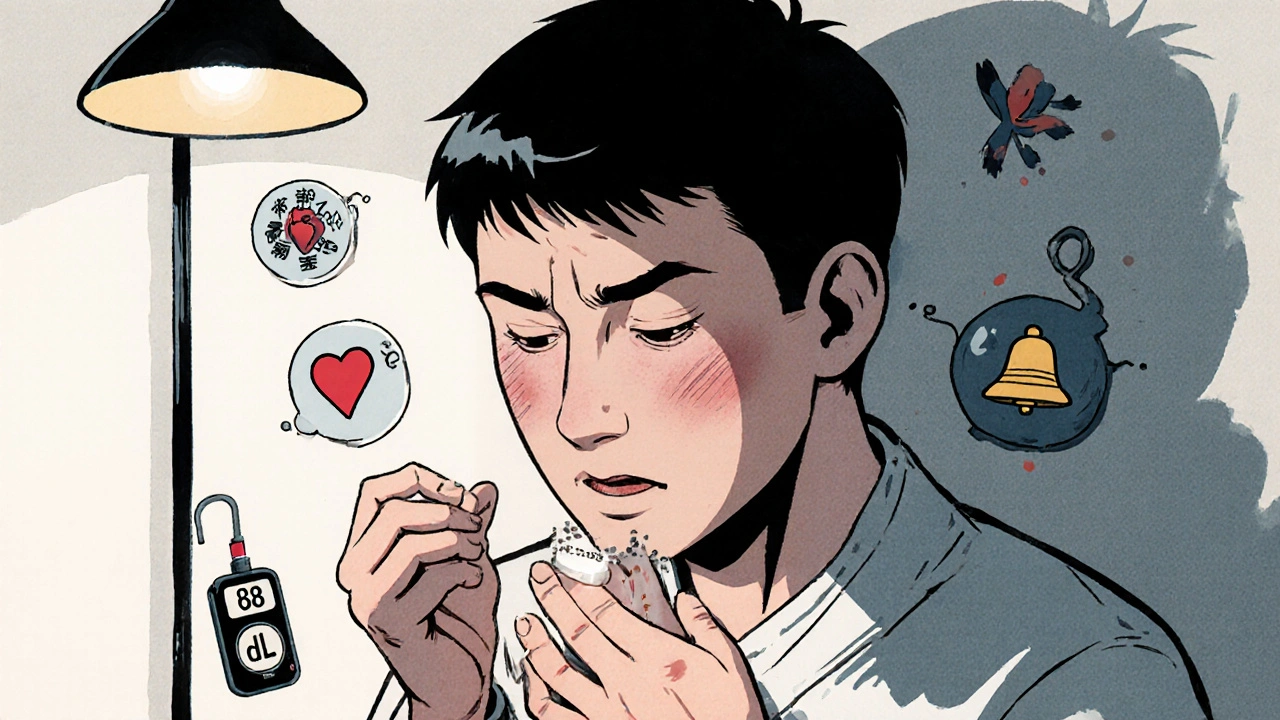
When you start insulin therapy, it’s not just about getting your blood sugar under control. It’s about learning to live with two very real, very common side effects: hypoglycemia and weight gain. For many people with type 1 or advanced type 2 diabetes, insulin is life-saving. But it’s also the most likely cause of dangerous low blood sugar and unwanted pounds. And while doctors focus on A1c numbers, the real struggle happens in the quiet moments-when your hands shake, your heart races, or you stare at the scale wondering why you’re gaining weight even though you’re eating less.
What Hypoglycemia Really Feels Like
Hypoglycemia isn’t just a number on a glucose meter. It’s a full-body alarm. When your blood sugar drops below 70 mg/dL (3.9 mmol/L), your body goes into survival mode. You might feel dizzy, sweaty, or suddenly hungry. Your heart pounds. Your vision blurs. Your words come out jumbled. In severe cases, you pass out. And if no one’s around? That’s when it turns dangerous. Studies show that people on intensive insulin therapy have three times the risk of severe hypoglycemia compared to those on looser control. In type 1 diabetes, that’s about 2 to 3 serious low-blood-sugar events per person every year. And it’s not just about feeling bad-it’s about the long-term damage. Severe episodes can trigger heart stress, brain fog, and even increase the risk of car crashes. One study found that 25% of people with type 1 diabetes lose their warning signs after 15 to 20 years. That’s called hypoglycemia unawareness. You don’t feel the warning. You just wake up with a headache-or worse, find yourself in the hospital.Why Insulin Makes You Gain Weight
Insulin doesn’t just move glucose into your cells. It tells your body to store it. As fat. Before insulin therapy, your body was losing sugar through urine. That’s calories-up to 400 a day-just floating away. Once you start insulin, that stops. Every gram of glucose that used to be flushed out now gets stored as glycogen or fat. On top of that, insulin blocks fat breakdown. It’s an anabolic hormone. It builds things up. That’s good for muscle and tissue repair. Not so good if you’re trying to avoid gaining 4 to 6 kilograms in the first year. It’s not just about calories in, calories out. It’s about biology. Even if you eat the same amount, insulin changes how your body uses it. And many people, scared of lows, end up eating more snacks to stay safe. That’s a cycle: fear of low blood sugar → extra carbs → higher insulin dose → more fat storage → more weight → harder to control blood sugar.The Trade-Off: Better Control, Higher Risk
The Diabetes Control and Complications Trial (DCCT) proved one thing clearly: tight blood sugar control slashes your risk of blindness, kidney failure, and nerve damage by 76%. But it also tripled the chance of severe hypoglycemia. That’s the brutal trade-off. Doctors used to push everyone toward an A1c under 7%. Now, guidelines have changed. For older adults, people with heart disease, or those who’ve had frequent lows, the target might be 7.5% to 8%. Why? Because the harm from a single severe low can outweigh the benefit of a lower A1c. It’s not about perfection. It’s about safety. And weight gain? It’s not inevitable. But it’s common. Studies show that without any lifestyle changes, the average person gains 6.2 kg in the first year on insulin. With early dietary counseling and activity planning? That drops to 2.8 kg. The difference isn’t magic. It’s structure.
How to Prevent Hypoglycemia
You can’t eliminate low blood sugar-but you can drastically reduce it.- Check your blood sugar 4 to 6 times a day. Don’t skip meals or workouts without testing.
- Use continuous glucose monitoring (CGM). It’s not just for tech lovers. It alerts you before you crash. In trials, CGMs cut hypoglycemia by 40-50%.
- Learn your insulin-to-carb ratio and correction factor. Guessing doses is how most lows happen.
- Carry fast-acting sugar everywhere. Glucose tabs. Juice. Candy. Not chocolate-it’s too slow.
- Tell someone close to you how to give a glucagon injection. If you pass out, they’re your lifeline.
- Wear a medical bracelet. It’s simple. It’s cheap. And it can save your life.
How to Manage Weight Gain
Weight gain on insulin isn’t a personal failure. It’s a biological side effect. But it’s manageable.- Work with a dietitian. Don’t just eat “healthy.” Learn portion control and timing. Insulin works best when carbs are consistent.
- Choose low-glycemic foods. Whole grains, legumes, non-starchy vegetables. They don’t spike your blood sugar, so you need less insulin.
- Move daily. Even 30 minutes of walking lowers insulin resistance and helps burn stored fat.
- Don’t treat every low with a full juice box. Use 15 grams of glucose-just enough to raise your sugar, not flood your system.
- Ask about combination therapy. GLP-1 agonists like semaglutide (Ozempic, Wegovy) are now often paired with insulin. They reduce appetite, lower blood sugar, and help you lose weight. In trials, people lost 5 to 10 kg over 30 weeks.
New Tools Making a Difference
The last decade brought real progress. Newer insulins like insulin degludec (Tresiba) and insulin glargine U300 (Toujeo) have flatter, longer action. They cause 20-40% fewer nighttime lows than older NPH insulin. That’s huge for safety. Closed-loop systems-sometimes called artificial pancreases-automatically adjust insulin based on real-time glucose readings. In trials, they reduced time spent in hypoglycemia by 72%. They’re not perfect. They’re expensive. But for those who can access them, they’re life-changing. And the future? It’s not just about better drugs. It’s about smarter care. Programs that start nutrition and exercise counseling the day you begin insulin. Apps that track patterns and suggest adjustments. Teams that include mental health support-because fear of lows can be paralyzing.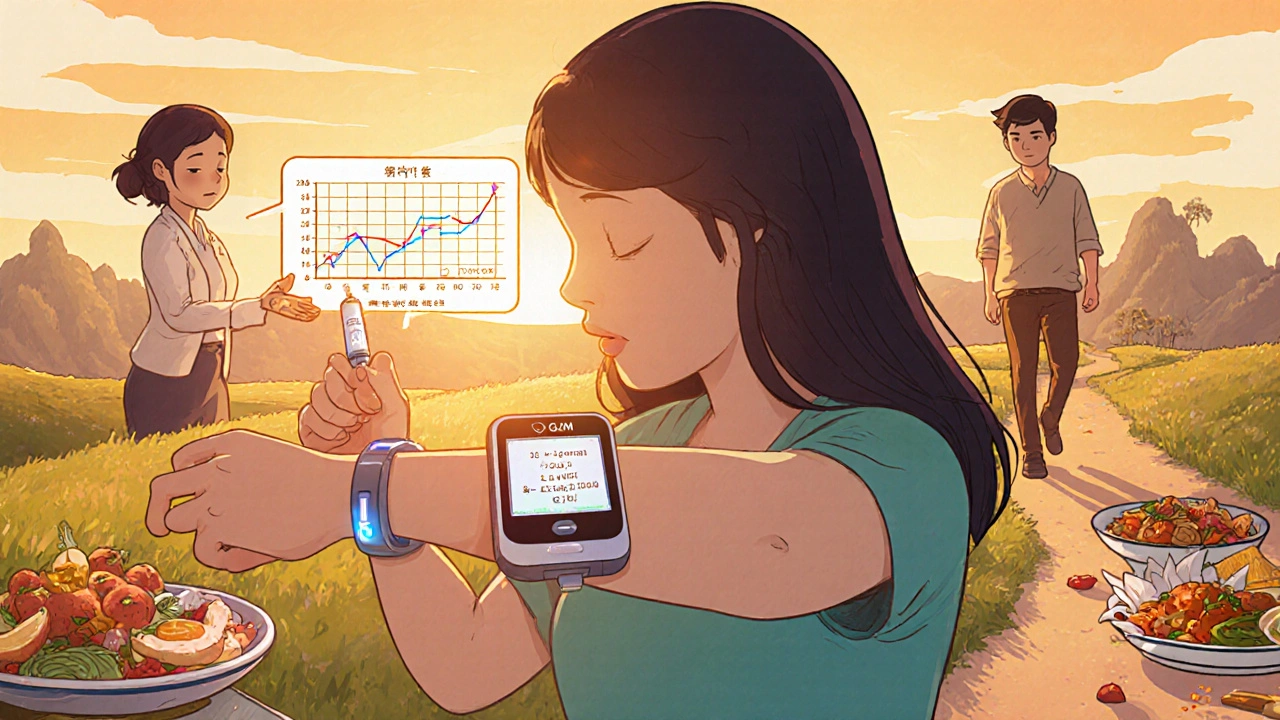
What Patients Don’t Talk About
Many people with diabetes admit they skip insulin doses to avoid weight gain. One study found 15-20% intentionally underdose. That’s not rebellion. It’s survival. But it’s dangerous. High blood sugar damages nerves, kidneys, eyes. The weight gain is visible. The damage isn’t. Others avoid exercise because they’re scared of lows. They cancel plans. They stop going out. The emotional toll is real. Anxiety, depression, guilt-it’s part of the package. The key is not to fight the side effects alone. Talk to your care team. Ask about CGMs. Ask about GLP-1 combinations. Ask for a referral to a diabetes educator. You’re not weak for struggling. You’re human.Final Thought: Balance, Not Perfection
Insulin therapy isn’t about reaching a perfect number. It’s about living well. That means controlling your blood sugar without living in fear. Gaining control without gaining weight. Finding a rhythm that works for your life-not just your lab results. The goal isn’t to eliminate side effects. It’s to manage them so they don’t control you.Can insulin cause you to pass out?
Yes. Severe hypoglycemia from insulin can cause unconsciousness, especially if blood sugar drops below 50 mg/dL (2.8 mmol/L). This is a medical emergency. If someone is unconscious and you don’t have glucagon, call emergency services immediately. Do not try to give them food or drink-they could choke.
Why do I gain weight even though I’m eating less?
Insulin stops your body from losing glucose through urine, which means you’re no longer burning off extra calories. It also promotes fat storage and blocks fat breakdown. Even if you eat less, your body is now more efficient at storing energy as fat. That’s why weight gain is common when starting insulin-even with careful eating.
Is it safe to skip insulin doses to avoid weight gain?
No. Skipping insulin leads to high blood sugar, which causes long-term damage to your eyes, kidneys, nerves, and heart. While weight gain is frustrating, the risks of uncontrolled diabetes are far more serious. Talk to your doctor about alternatives like GLP-1 agonists or insulin regimens that are less likely to cause weight gain.
Can continuous glucose monitors (CGMs) help with both lows and weight gain?
Yes. CGMs help you catch lows before they happen, so you don’t need to over-treat with extra carbs. That means fewer unnecessary calories. They also show how food and activity affect your blood sugar, helping you fine-tune meals to reduce insulin spikes and cravings. Many people find that using a CGM helps them lose weight simply by making smarter choices.
What’s the best way to treat a low blood sugar episode?
Use 15 grams of fast-acting glucose: 3-4 glucose tablets, 4 ounces of juice, or 1 tablespoon of sugar or honey. Wait 15 minutes, then check your blood sugar again. If it’s still low, repeat. Once your sugar is back up, eat a small snack with protein or complex carbs if your next meal isn’t for more than an hour. Avoid chocolate or candy bars-they’re too slow and full of fat, which delays sugar absorption.
Do newer insulins cause less weight gain?
Not directly. Newer insulins like degludec and glargine U300 are designed to reduce hypoglycemia, not weight gain. But by lowering the risk of lows, you’re less likely to overeat to prevent them. That indirect effect can help manage weight. For actual weight loss, combining insulin with GLP-1 agonists is far more effective.
Oh please. Another 'insulin is a burden' sob story. In India, we don't have the luxury of CGMs or GLP-1 agonists. We're lucky if we get insulin at all, let alone 'flatter, longer-acting' brands. Your first-world problems are nauseating. People here are dying because they skip doses to afford food, not because they 'gained 6 kg.' Stop romanticizing your metabolic struggles as if they're a tragic opera.
And yes, I'm aware you think your 'biological reality' is unique. It's not. It's just privilege with a glucose meter.