Cycle & Ovulation Tracker
Track Your Cycle & Ovulation
Enter your menstrual cycle information to estimate ovulation window and assess regularity.
Ovulation Results
Next Period
Ovulation Window
When it comes to managing ovulation and keeping your menstrual cycle on track, regular gynecological check‑ups are a cornerstone of reproductive health. These appointments give doctors a chance to look at your hormonal balance, spot early signs of disorders, and guide lifestyle tweaks that keep cycles predictable.
What Counts as a Regular Gynecological Check‑Up?
A "regular" visit usually means an exam once a year if you have no known issues, or every six months if you’re dealing with conditions like PCOS. The goal isn’t just a quick glance; it’s a comprehensive review of everything that influences ovulation and menstruation.
How Check‑Ups Influence Ovulation and Hormonal Balance
Ovulation is the release of an egg from the ovary, driven by a finely tuned hormone orchestra. Any disruption-stress, thyroid problems, or a hidden infection-can throw the rhythm off.
During a check‑up, clinicians assess hormonal balance by measuring estrogen, progesterone, LH, and FSH levels. When these numbers are in the right range, the body signals the ovary to release an egg at the expected time, leading to regular periods.
Key Components of the Visit
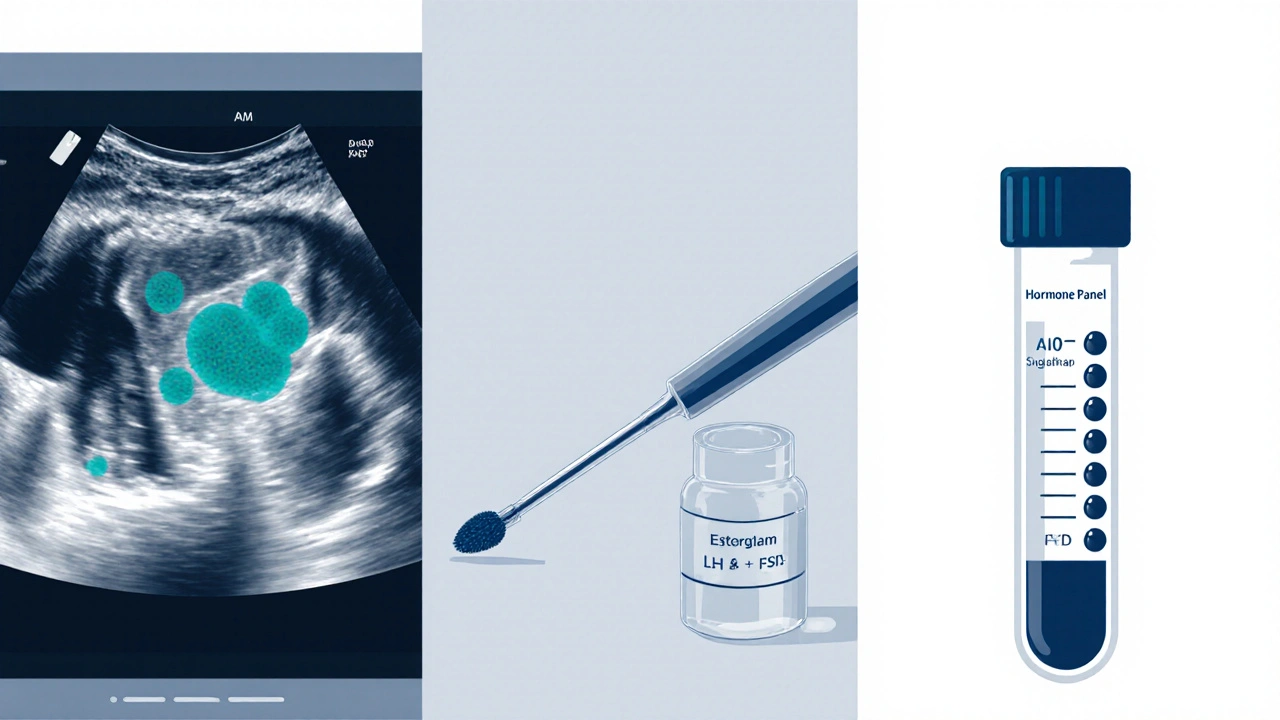
Most appointments include three core elements that directly affect cycle regularity:
- Pap smear - screens for cervical changes that could indirectly affect hormone production.
- Pelvic ultrasound - visualizes ovarian follicles, showing whether they’re developing correctly each cycle.
- Hormone panel - a blood test that quantifies key hormones, flagging imbalances before they cause missed periods.
Below is a quick side‑by‑side look at what a standard visit includes compared with a fertility‑focused session.
| Aspect | Standard Check‑Up | Fertility‑Focused Visit |
|---|---|---|
| Duration | 15‑20 minutes | 30‑45 minutes |
| Tests Included | Pap smear, basic blood work | Ultrasound, comprehensive hormone panel, AMH test |
| Typical Cost (NZD) | ~$80‑$120 | ~$250‑$400 |
| Follow‑up Frequency | Annual | Every 3‑6 months if trying to conceive |
When to Schedule an Appointment - Signs You Shouldn’t Ignore
Even if you’re on an annual schedule, certain symptoms merit an earlier visit:
- Sudden changes in cycle length (e.g., from 28 to 40 days)
- Heavy or very light bleeding lasting more than seven days
- Painful periods that disrupt daily life
- Unexplained weight gain or loss
- Persistent fatigue or mood swings
These clues often point to underlying conditions such as Polycystic ovary syndrome (PCOS) or Endometriosis, both of which can throw off ovulation.
Preparing for Your Visit and Making the Most of It
To get the most value from your appointment, bring a few items:
- A menstrual diary covering the last three cycles (dates, flow, symptoms)
- A list of all medications and supplements you take
- Questions about birth control, fertility plans, or any pain you’ve felt
During the exam, don’t hesitate to ask for clarification on test results. A good clinician will explain what each hormone reading means for your cycle and suggest concrete actions.
Common Concerns: PCOS, Endometriosis, and Irregular Periods
PCOS affects roughly 1 in 7 women of reproductive age. It’s characterized by elevated androgen levels, insulin resistance, and multiple ovarian cysts. Regular monitoring can catch hormone spikes early, allowing diet changes or medication to restore regular ovulation.
Endometriosis involves tissue similar to the uterine lining growing outside the uterus, leading to painful periods and sometimes infertility. Early detection through ultrasound and laparoscopy improves treatment success.
Both conditions benefit from a tailored fertility assessment that measures anti‑Müllerian hormone (AMH) levels, an indicator of ovarian reserve.
DIY Tips to Support Cycle Regularity Between Visits
While doctors handle the heavy lifting, you can keep things running smoothly with a few everyday habits:
- Track your temperature each morning; a slight rise signals ovulation.
- Maintain a balanced diet rich in omega‑3 fatty acids, leafy greens, and whole grains - these support hormone production.
- Aim for 7‑9 hours of sleep; chronic sleep loss disrupts the hypothalamic‑pituitary‑ovarian axis.
- Manage stress with mindfulness, yoga, or regular walks; cortisol spikes can suppress ovulation.
- Limit caffeine and alcohol, both of which can alter estrogen metabolism.
Even modest tweaks can make a noticeable difference, especially when coupled with routine check‑ups.
The Bottom Line
Keeping an eye on your reproductive system isn’t a luxury - it’s a practical strategy for smoother cycles, better fertility odds, and overall health. By staying on top of regular gynecological check-ups, you give your body the feedback loop it needs to fine‑tune ovulation and keep menstruation on schedule.
Frequently Asked Questions
How often should I have a gynecological check‑up if I have regular periods?
For most women with a stable 28‑day cycle and no underlying conditions, an annual visit is sufficient. The doctor will review your history, perform a pelvic exam, and possibly order a basic hormone panel if you’re over 35.
Can a pap smear affect my fertility?
A pap smear itself doesn’t impact fertility. However, it can detect cervical abnormalities that, if left untreated, might cause inflammation and indirectly affect hormone signaling.
What does an ultrasound show about ovulation?
A transvaginal ultrasound tracks follicle growth. When a follicle reaches about 18‑24mm, it’s ready to release an egg. Seeing this pattern over a few cycles helps the doctor confirm whether ovulation is occurring regularly.
I have irregular periods but don’t want to get pregnant right now. Should I still see a doctor?
Yes. Irregular cycles can signal hormonal imbalances, thyroid issues, or early signs of PCOS. Early diagnosis lets you address the root cause, reducing the risk of future complications and improving overall well‑being.
Are there any risks to frequent gynecological visits?
The procedures involved-pelvic exams, pap smears, ultrasounds-are low‑risk. The biggest consideration is comfort; choose a provider you trust and communicate any concerns before the exam.

Regular check‑ups help catch issues early.