Medication Risk Checker for Hyperkalemia
Hyperkalemia Risk Assessment
Check your risk of dangerous hyperkalemia (blood potassium >5.5 mEq/L) based on medications and health factors
Enter Your Medications
Risk Assessment
What Is Hyperkalemia and Why Should You Care?
Hyperkalemia means your blood potassium is too high - above 5.5 mEq/L. At first, you might not feel anything. No swelling. No pain. Just quiet, creeping danger. But when potassium climbs past 6.5 mEq/L, your heart starts to misfire. Peaked T-waves on an ECG. Slowed signals. Wider QRS complexes. Then, if nothing’s done, ventricular fibrillation. Sudden cardiac arrest. This isn’t theoretical. It happens in hospitals every day, often because of medicines people take daily for high blood pressure, heart failure, or kidney disease.
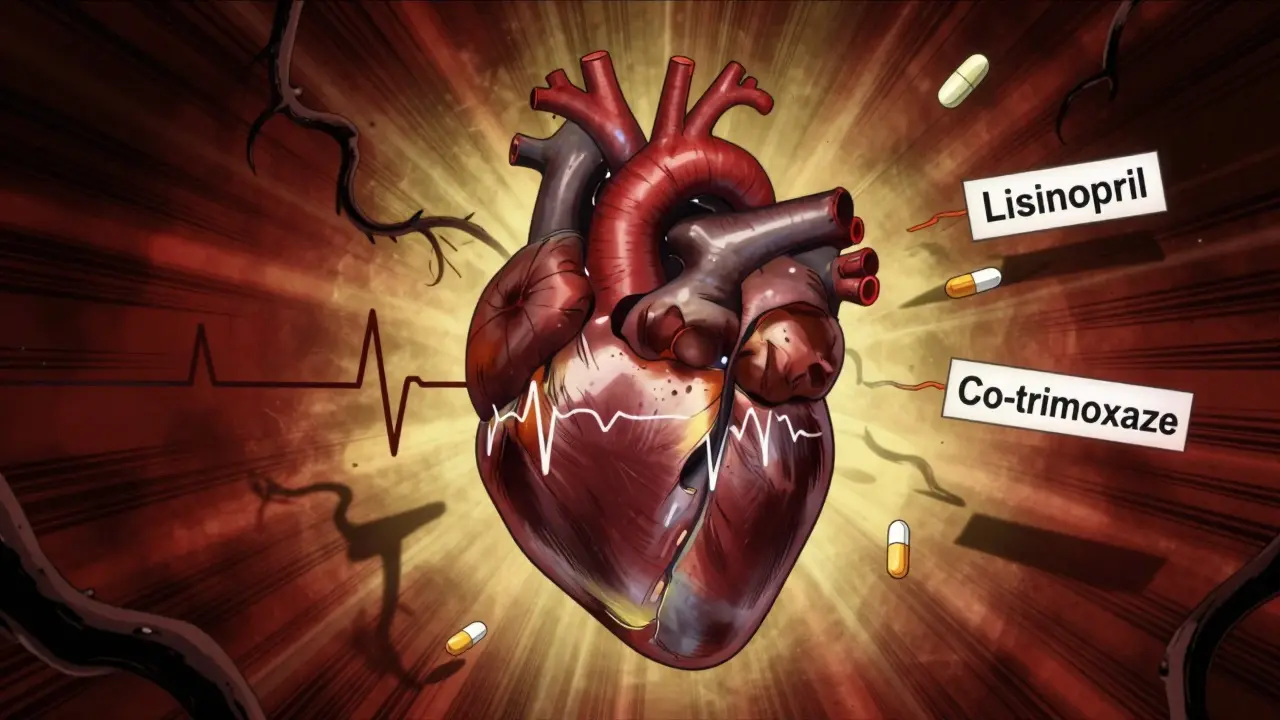
Which Medications Cause This?
The usual suspects aren’t obscure drugs. They’re the ones doctors prescribe because they save lives. ACE inhibitors like lisinopril. ARBs like losartan. Spironolactone, a water pill that keeps potassium in. Even aliskiren, a newer renin blocker. These drugs work by blocking the body’s natural way of flushing out potassium. That’s good for your heart and kidneys - until it’s not.
Here’s the real problem: combining them. Taking spironolactone with an ACE inhibitor? That’s risky. Add co-trimoxazole (an antibiotic) into the mix? Risk jumps 5.5 times. That’s not a small increase. That’s a red flag. People with kidney disease, diabetes, or over 65 are at highest risk. Dehydration makes it worse. Even skipping a dose of your diuretic can push potassium up.
How Your Heart Pays the Price
Your heart beats because of tiny electrical signals. Potassium helps control those signals. Too much potassium? The electrical system gets confused. Cells can’t reset properly. The result? Arrhythmias. Palpitations. Fluttering in your chest. Sometimes it’s subtle - you just feel tired or weak. Other times, it’s sudden. No warning. That’s why hyperkalemia is called a silent killer.
At 5.5 mEq/L, ECG changes start. By 6.0 mEq/L, doctors see clear signs: tall, narrow T-waves. At 7.0 mEq/L, the QRS complex widens. The heartbeat slows. Then comes the sine wave pattern - a final warning before the heart stops beating in rhythm. This isn’t a slow decline. It’s a race against time. And if you’re on RAAS inhibitors (those blood pressure meds), you’re already at higher risk. The very drugs protecting your heart can also be the ones putting it in danger.
What Happens in an Emergency?
If potassium hits 6.5 mEq/L or higher - or if ECG changes show up - you need immediate treatment. Not tomorrow. Not in an hour. Now.
First, give calcium gluconate. Not to lower potassium. To protect the heart. It stabilizes the heart muscle’s electrical activity. Effects kick in within minutes. You won’t feel better, but your heart will be safer. Next, shift potassium into cells. Give insulin with glucose - 10 units of insulin and 25 grams of sugar. That drops potassium by 0.5 to 1.5 mEq/L in 15 to 30 minutes. Nebulized albuterol helps too. It pushes potassium into cells and works fast.
These are emergency moves. They buy time. But they don’t fix the root problem. You still need to remove the extra potassium from your body.
Long-Term Fixes: Potassium Binders Are a Game Changer
For years, the only option was to stop the life-saving meds. But that’s not a solution. Stopping an ACE inhibitor or spironolactone increases the risk of heart failure, stroke, and death. Now, we have better tools: potassium binders.
Patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) are oral powders that trap potassium in the gut. They don’t get absorbed. They just collect it and carry it out in stool. Within hours, potassium drops by 0.4 to 1.0 mEq/L. Studies show 86% of patients can stay on their RAAS inhibitors when using these binders. Without them, nearly 40% of patients had to lower or stop their meds just because of mild hyperkalemia.
Side effects? Constipation in 15-20%. Diarrhea in 10-15%. Not fun, but far better than a heart attack. These aren’t experimental. They’re FDA-approved. Used daily. Prescribed by cardiologists and nephrologists. And they’re changing how we treat chronic kidney disease and heart failure.
What You Can Do Right Now
If you’re on any of these meds - ACE inhibitors, ARBs, spironolactone, or eplerenone - get your potassium checked every 1 to 4 weeks, especially if you have kidney issues. Don’t wait for symptoms. Most people have none until it’s too late.
Watch your diet. Bananas, oranges, potatoes, spinach, tomatoes, and salt substitutes with potassium chloride can push levels up. Aim for 2,000 to 3,000 mg of potassium daily. That’s not zero. It’s just mindful. Talk to a dietitian. Most patients never get this advice.
Don’t take over-the-counter potassium supplements unless your doctor says so. And avoid NSAIDs like ibuprofen - they hurt kidney function and raise potassium.
If you feel dizzy, weak, or your heart races, get checked. Don’t assume it’s stress. It might be your potassium.
The Bigger Picture: Staying on Life-Saving Meds
The goal isn’t to avoid hyperkalemia at all costs. It’s to manage it so you can keep taking the drugs that keep you alive. RAAS inhibitors reduce heart failure deaths by 20-30%. They slow kidney disease progression. Stopping them because of a high potassium reading is like turning off your smoke alarm because it goes off once.
Modern medicine now gives us a third option: don’t stop. Don’t lower the dose. Don’t hope it fixes itself. Bind the potassium. Monitor closely. Stay on therapy. That’s the new standard. And it’s working.
By 2025, more than half of patients with chronic kidney disease and heart failure on RAAS inhibitors are using potassium binders. The old days of discontinuing these drugs are fading. The future is about control - not avoidance.
When to Call Your Doctor
Call immediately if:
- You have chest pain, palpitations, or irregular heartbeat
- You feel unusually weak, tired, or numb
- You’re vomiting or have diarrhea and can’t keep fluids down
- Your ECG shows new changes and you’re on a RAAS inhibitor
Don’t wait for your next appointment. Hyperkalemia doesn’t wait.
I had no idea potassium could be this sneaky. My grandma’s on lisinopril and spironolactone, and she’s always been fine-until last month she got dizzy and weak. Turned out her potassium was 6.8. Scary how quiet it is until it’s not. Glad I’m checking her labs now.