Statin Tolerance Genetic Checker
Statin Tolerance Assessment
This tool helps you understand your genetic risk for statin-related muscle pain. Based on your SLCO1B1 genotype, it will recommend the safest statin options for you.
Personalized Statin Recommendations
Your Risk Level
Recommendations
Why Some People Can’t Tolerate Statins-And How Genetics Might Hold the Answer
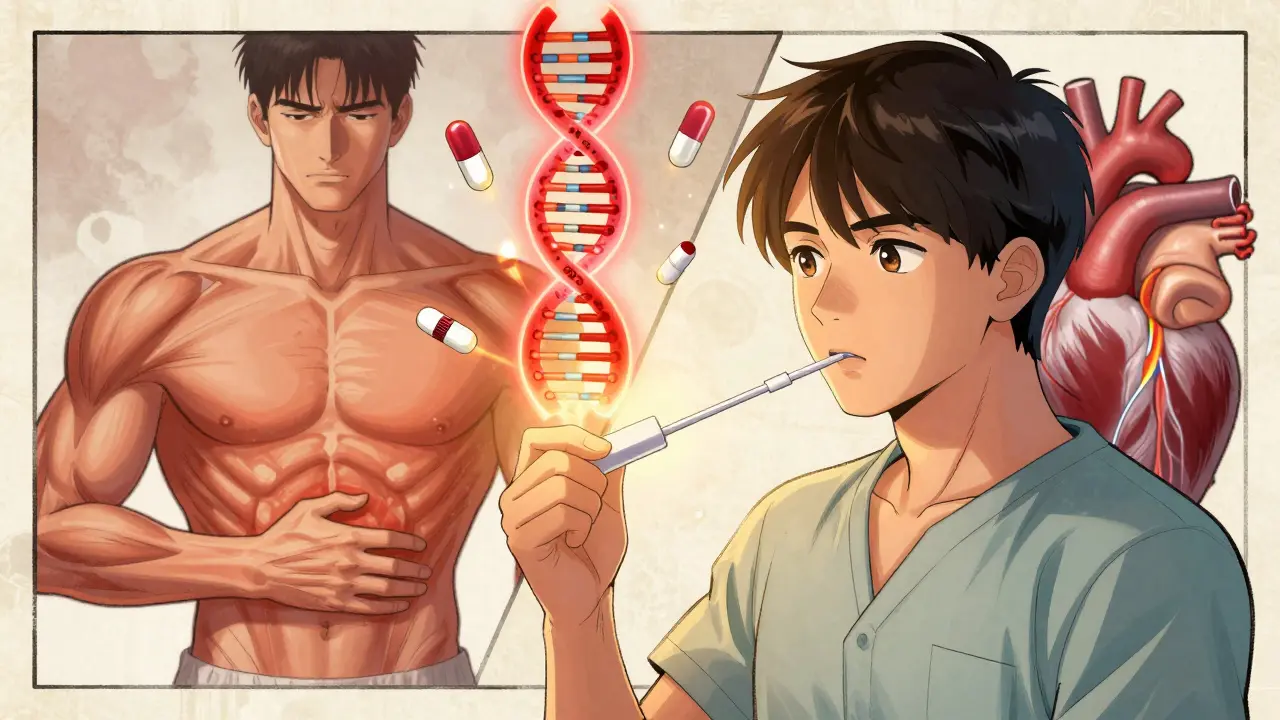
Statins are one of the most prescribed drugs in the world. Millions take them every day to lower cholesterol and prevent heart attacks. But for a significant number of people, these drugs cause muscle pain, weakness, or cramps-so bad they have to stop taking them. This isn’t just bad luck. For many, it’s written in their DNA.
The key lies in a single gene: SLCO1B1. This gene makes a protein that pulls statins out of the bloodstream and into the liver, where they’re meant to work. But if you have a specific version of this gene-called the c.521T>C variant-your body doesn’t clear statins properly. That means the drug builds up in your muscles, causing damage. People with two copies of this variant (CC genotype) are nearly five times more likely to get severe muscle injury on high-dose simvastatin than those with no copies (TT genotype). Even one copy (TC) doubles the risk.
Not All Statins Are Created Equal
It’s easy to assume all statins act the same. They don’t. The SLCO1B1 gene issue matters most for simvastatin-especially at the 80 mg dose. For atorvastatin and rosuvastatin, the same genetic variant barely moves the needle. A 2021 study of nearly 12,000 people found no link between SLCO1B1 and muscle symptoms with these two statins.
This matters because it changes your options. If you’ve had muscle pain on simvastatin and tested positive for the CC variant, switching to pravastatin or fluvastatin often solves the problem. These statins don’t rely as heavily on the SLCO1B1 transporter. One study showed pravastatin caused 80% fewer muscle issues in CC carriers compared to simvastatin. That’s not a small difference-it’s life-changing for someone who thought they’d never be able to take a statin again.
What Else Is in Your DNA That Might Affect Statin Tolerance?
SLCO1B1 is the biggest player, but it’s not the only one. Other genes play smaller roles. CYP2D6 and CYP3A4 help break down certain statins. If you’re a slow metabolizer because of a genetic variant, those drugs stick around longer, raising your risk of side effects. Then there’s ABCB1 and ABCG2-genes that control how statins are pumped out of cells. If those aren’t working right, statins can accumulate where they shouldn’t.
More recent research has flagged two other genes: GATM and CACNA1S. These were linked to muscle symptoms in large genome studies, but their exact roles are still unclear. Even newer is SOAT1, which showed a strong statistical link in a 2021 study-but no one knows yet how it affects muscle tissue. The takeaway? Your risk isn’t just about one gene. It’s a mix of small effects adding up.
Who Should Get Tested-and When?
The big question: Should everyone get tested before starting a statin? Not yet. Guidelines from the Clinical Pharmacogenetics Implementation Consortium (CPIC) say testing is most useful for people who’ve already had muscle symptoms and are considering trying simvastatin again. If you’ve never had trouble, testing upfront isn’t routinely recommended.
But here’s where it gets practical: If you’ve been told you’re statin-intolerant, testing can open doors. A Mayo Clinic survey found that 78% of people who’d previously stopped statins due to muscle pain were able to restart one safely after genetic testing guided the choice. That’s a huge win for someone who needs to lower their cholesterol to avoid a heart attack.
Some doctors now test before the first prescription-especially in high-risk patients like those with family history of early heart disease. This is called pre-emptive testing. One study showed it boosted statin adherence by nearly 20% compared to waiting until problems showed up.
The Reality of Getting Tested
Getting tested is easier than ever. Most labs offer it via a simple cheek swab. Results come back in about a week. Companies like Mayo Clinic, ARUP, and Color Genomics provide detailed reports with clear dosing advice based on your genotype.
But here’s the catch: Insurance doesn’t always pay. As of 2022, only about 28% of commercial insurers covered SLCO1B1 testing. Out-of-pocket costs can range from $150 to $400. Medicare only covers it in very specific cases. That’s a barrier for many.
And even if you get the results, your doctor might not know what to do with them. A 2021 survey found that 34% of primary care doctors felt unprepared to interpret pharmacogenomic reports. That’s why tools built into electronic health records-like Epic and Cerner-are so important. They can pop up alerts when a doctor tries to prescribe simvastatin 80 mg to someone with a CC genotype, suggesting safer alternatives automatically.
What the Evidence Really Says
There’s a gap between what the science says and what happens in real life. On one hand, experts like Dr. Julie Johnson call SLCO1B1 testing the strongest example of pharmacogenomics in cardiovascular care. The evidence is solid. On the other hand, a 2020 Harvard study found that giving doctors genetic results didn’t improve patient adherence or reduce muscle symptoms. Why? Because many patients still had symptoms from other causes-like low vitamin D, thyroid issues, or simply aging muscles.
SLCO1B1 only explains about 6% of all statin-related muscle complaints. That means most people who have symptoms don’t have this gene variant. So testing won’t help everyone. But for the ones it does help? It can be everything.
What’s Next for Genetic Testing and Statins?
Researchers are now moving beyond single genes. The future is in polygenic risk scores-combining data from 10, 15, even 20 different genetic markers to predict risk more accurately. Early studies show these scores can improve prediction from 58% to 67% accuracy. That’s still not perfect, but it’s progress.
More healthcare systems are starting to offer pre-emptive pharmacogenomic testing. The Statin Pharmacogenomics Implementation Consortium is working to standardize testing across 50 U.S. hospitals by 2025. And as costs drop and evidence grows, coverage will likely improve.
For now, if you’ve been told you can’t take statins because of muscle pain, don’t give up. Ask your doctor about genetic testing. It might not be the whole answer-but for some people, it’s the missing piece that lets them take control of their heart health again.
Can genetic testing tell me if I’ll get muscle pain from statins?
Yes-but only partially. The SLCO1B1 gene variant c.521T>C is the strongest known genetic predictor of muscle pain with simvastatin. People with two copies of the C allele (CC genotype) have up to a 4.5-fold higher risk. But this gene only explains about 6% of all statin-related muscle symptoms. Many other factors-like age, thyroid function, vitamin D levels, and other medications-also play a role. So a negative test doesn’t guarantee you won’t have side effects, and a positive test doesn’t mean you definitely will.
Which statins are safest if I have the SLCO1B1 gene variant?
If you have the CC genotype, avoid high-dose simvastatin (80 mg) entirely. Lower doses (20 mg or less) may still be okay, but switching is often better. Pravastatin and fluvastatin are the safest alternatives because they don’t rely heavily on the SLCO1B1 transporter to enter the liver. Rosuvastatin and atorvastatin are also generally safe for CC carriers, since their metabolism follows different pathways. Studies show pravastatin causes 80% fewer muscle issues in CC carriers compared to simvastatin.
Is pharmacogenomic testing covered by insurance?
Coverage is inconsistent. As of 2022, only about 28% of commercial insurers in the U.S. covered SLCO1B1 testing. Medicare covers it only under very specific circumstances through its Molecular Diagnostic Services Program. Out-of-pocket costs range from $150 to $400 for standalone tests. Some larger health systems offer testing as part of broader pharmacogenomic panels, which may be covered under preventive benefits. Always check with your insurer before testing.
Should I get tested before my first statin prescription?
Current guidelines don’t recommend routine testing for everyone starting a statin. But pre-emptive testing may be worth considering if you have a strong family history of early heart disease, or if you’re at high risk for statin intolerance (e.g., older age, small body size, taking multiple medications). A 2021 study showed pre-emptive testing increased statin adherence by nearly 19% compared to waiting until side effects occurred. Talk to your doctor about whether it makes sense for your situation.
What if I test positive but still get muscle pain on a different statin?
That’s more common than you might think. SLCO1B1 only explains a small part of the picture. Muscle pain can come from other causes: low vitamin D, hypothyroidism, kidney issues, or even overexertion. Some people have multiple small genetic factors that add up. Others react to statins for reasons we don’t yet understand. If you still have symptoms after switching statins, your doctor should check for these other causes before giving up on statin therapy altogether.
Wow, this is exactly the kind of info I wish my doctor had shared when I stopped simvastatin three years ago. I thought I was just 'too sensitive'-turns out it was my DNA. Switched to pravastatin and haven’t had a single cramp since. If you’ve been told you’re statin-intolerant, don’t give up. Ask for the test. It’s not magic, but it’s close.