Why You Need a Medication Expiration Review Schedule
Most people don’t think about their medicine until they need it. But if you’ve ever opened a medicine cabinet and found a bottle of pills from 2019, you know how easy it is to forget. And that’s dangerous. Expired medications can lose potency, or worse - they can break down into harmful substances. The FDA says proper medication management could prevent 125,000 deaths a year in the U.S. alone. You don’t need to be a pharmacist to keep your meds safe. You just need a simple, regular system.
Think about it: if you take blood pressure pills, insulin, or an epinephrine auto-injector, the difference between a working dose and a useless one isn’t just inconvenient - it’s life or death. Even common meds like antibiotics or birth control pills can become ineffective after their expiration date. And if you’re storing them in a hot bathroom or a sunlit drawer? They degrade faster.
What Counts as an Expiration Date - and What Doesn’t
The date on your medicine bottle isn’t a "use-by" label. It’s a guarantee. The manufacturer tested that pill, liquid, or patch to make sure it still works as intended up to that date. After that? They can’t say for sure. The FDA requires all prescription and over-the-counter drugs to have an expiration date based on stability testing. But here’s the twist: many drugs last way longer than that date if stored properly.
A 2015 Mayo Clinic study found that 90% of tested drugs were still effective 15 years past their expiration - if kept cool, dry, and dark. The military’s Shelf Life Extension Program found similar results. But here’s the catch: you’re not the military. Your bathroom isn’t a climate-controlled warehouse. Humidity, heat, and light wreck medicine faster than you think. So while some pills might be fine, you shouldn’t gamble with critical drugs like nitroglycerin (for heart attacks), insulin, or liquid antibiotics. Those degrade fast. If they’re expired, throw them out.
How Often Should You Review Your Medications?
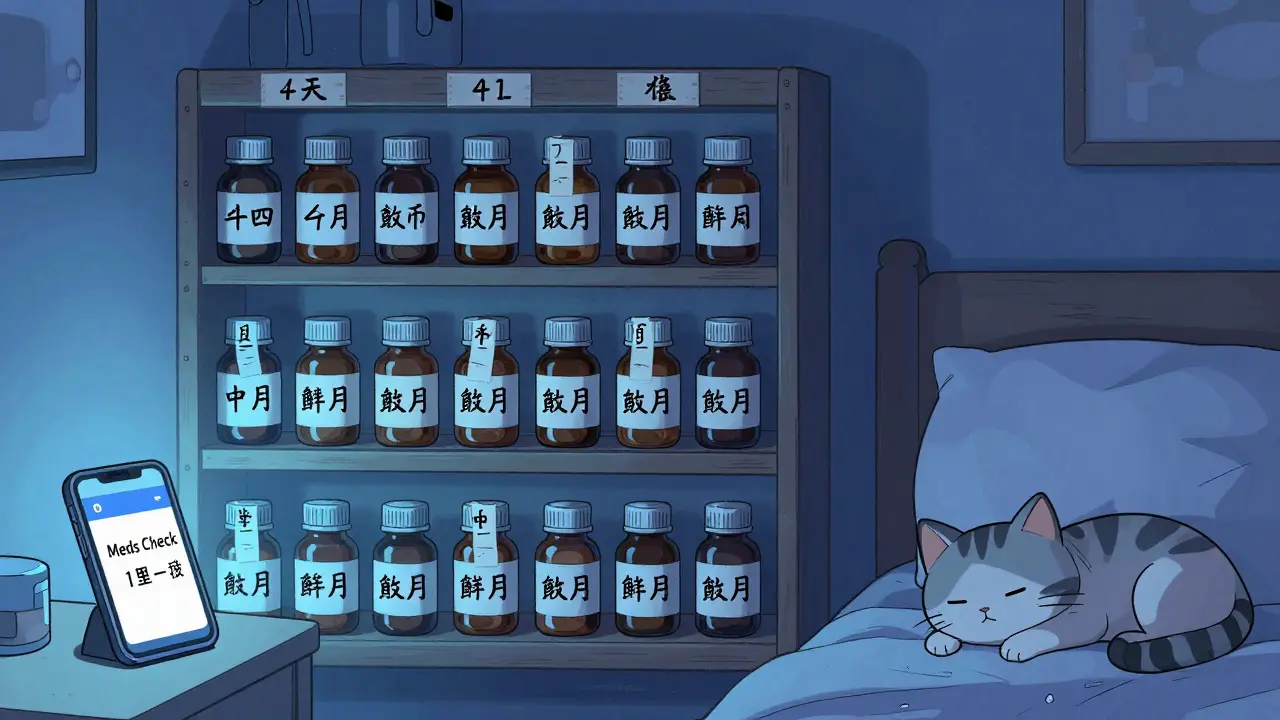
Not all meds need the same attention. The key is matching your review schedule to the risk. Here’s a simple breakdown:
- Monthly: Insulin, epinephrine pens, liquid antibiotics, and any meds stored in the fridge. These are high-risk and degrade quickly.
- Quarterly: Most pills, patches, and inhalers kept at room temperature. This includes blood pressure meds, thyroid pills, and pain relievers.
- Every six months: Emergency meds like asthma inhalers or epinephrine if they’re kept in a cool, dry place (like a bedroom drawer, not the car).
Set a calendar reminder. Pick a date that’s easy to remember - like the first Monday of every month. Make it a habit, like checking your smoke detector batteries. If you’re managing meds for someone else, like an aging parent, make it part of your weekly check-in.
How to Build Your Review System (Step by Step)
- Take everything out. Empty your medicine cabinet, purse, nightstand, and car glove box. Don’t skip the "emergency stash" - that’s where expired meds hide.
- Sort by type. Group pills, liquids, inhalers, patches, and injectables. Keep them in original containers. Never transfer meds to unlabeled containers - you’ll forget what’s inside.
- Check each expiration date. Look for the "EXP" or "Use by" date. If it’s printed tiny or faded, take a photo with your phone and label the bottle with a permanent marker. Seniors especially benefit from this - 48.7% of older adults struggle to read small print.
- Separate what’s expired. Put expired meds in a separate box. Don’t toss them in the trash or flush them. Use a take-back program. In New Zealand, pharmacies like Pharmacy Direct and Countdown offer free disposal bins. In the U.S., DEA’s National Prescription Drug Take Back Day happens twice a year.
- Record what’s left. Use a simple spreadsheet, a notebook, or an app. Write down: Drug name, strength, expiration date, storage location, and quantity. Apps like Medisafe or MedWise can auto-scan barcodes and send alerts. If you prefer paper, print a free template from the National Council on Aging.
- Set reminders. Use your phone calendar. Label entries as "Check: Amoxicillin - EXP 04/2026". Set alerts 1 week before expiration. For critical meds, set two alerts - one month out and one week out.
Storage Matters More Than You Think
Heat and moisture are the real enemies. The ideal storage temperature for most meds is 20-25°C (68-77°F). That’s not your bathroom. It’s a cool, dark drawer in your bedroom. Humidity from showers breaks down pills and patches. Sunlight fades labels and degrades liquids.
Refrigerated meds like insulin? Keep them in the fridge, but not in the door. The door gets warm every time you open it. Store them on a middle shelf. If you travel, keep insulin in a cooler bag with a cold pack - never in checked luggage.
Pro tip: If your meds smell weird, look discolored, or feel sticky, throw them out - even if the date hasn’t passed. That’s not expiration. That’s damage.
What to Do With Expired Medications
Never flush pills down the toilet. Never throw them loose in the trash. Both are dangerous for the environment and can be picked up by kids or pets.
Use a take-back program. In New Zealand, most pharmacies accept expired meds for safe disposal. In the U.S., visit DEA’s Take Back Day or find a permanent drop-off site near you. If that’s not possible, mix pills with coffee grounds or cat litter in a sealed bag before tossing. This makes them unappealing and unusable.
For sharps like needles or epinephrine pens: Use a hard plastic container (like a laundry detergent bottle), seal it, label it "SHARPS - DO NOT RECYCLE," and drop it at a pharmacy or hospital.
Real Problems People Face - And How to Fix Them
- "I can’t read the tiny print on the bottle." Use a magnifying glass or phone camera zoom. Write the date in big letters on masking tape and stick it to the bottle.
- "I’m scared to throw away expensive meds." Yes, insulin costs $300 a vial. But taking degraded insulin can land you in the hospital - that costs way more. Talk to your pharmacist. Some manufacturers offer patient assistance programs.
- "I forget to check." Tie it to another habit. "Every time I pay my electricity bill, I check my meds." Or set a recurring alarm on your phone labeled "Meds Check - 1st Monday".
- "My parent has 20 different bottles and doesn’t know what’s what." Use a pill organizer with date labels. Or better yet, get a smart dispenser like Hero Health. It dispenses pills automatically and alerts caregivers if a dose is missed.

What Works: Real Results
CVS Health tracked patients using their MedSchedule app for a year. Those users saw a 37.2% drop in expired medication incidents. In one nursing home, staff started weekly reviews. Within six months, medication errors dropped by 51%.
And it’s not just about safety - it’s about saving money. The Kaiser Family Foundation found Americans throw away $7.2 billion in unexpired meds every year because they’re confused. You don’t have to be one of them.
What to Do Next
Right now, open your medicine cabinet. Take out one bottle. Check the expiration date. If it’s expired, don’t wait. Don’t rationalize. Don’t think, "It still looks fine." If it’s past the date and it’s insulin, nitroglycerin, or a liquid antibiotic - toss it. If it’s a regular pill, mark it for disposal.
Then, pick one day next week. Set a 10-minute timer. Go through every bottle. Write down the dates. Set a reminder. That’s it. You’ve just started a system that could save your life - or someone else’s.
Can I still take medicine after the expiration date?
For most solid pills - like aspirin or blood pressure meds - yes, they may still work if stored properly. But for insulin, nitroglycerin, liquid antibiotics, and epinephrine, never use them past the date. They degrade fast and can fail when you need them most. When in doubt, throw it out.
How do I know if a medicine has gone bad?
Look for changes: pills that are cracked, discolored, or smell funny. Liquids that are cloudy, have particles, or smell off. Patches that are sticky or brittle. Inhalers that don’t spray properly. If anything looks or smells wrong - even if the date is fine - don’t use it.
What’s the difference between "expiration date" and "beyond use date"?
Expiration date is set by the manufacturer - it’s when they guarantee the drug works. Beyond Use Date (BUD) is set by the pharmacy when they repackage or compound a drug. BUDs are usually shorter - for example, a pill repackaged into a blister pack might have a BUD of 6 months, even if the original bottle says 2 years.
Should I use a phone app to track expiration dates?
Yes - especially if you take multiple meds. Apps like Medisafe, MedWise, or MyTherapy let you scan barcodes, set alerts, and even notify family members. They’re free or low-cost and reduce missed doses and expired meds by over 50% in studies.
Where can I safely dispose of expired medications in New Zealand?
Most pharmacies - including Pharmacy Direct, Countdown, and New World - have free take-back bins for expired or unwanted meds. You can also drop them off at your local hospital pharmacy. Never flush or trash them loose. Safe disposal protects the environment and prevents accidental poisoning.
Is it safe to keep old prescriptions "just in case"?
No. Medications are prescribed for specific conditions and dosages. Taking an old antibiotic for a new infection can lead to antibiotic resistance. Old painkillers won’t help a new injury if they’ve degraded. Always get a new prescription if you need it again.
Final Thought: Small Steps, Big Safety Net
You don’t need a fancy system. You don’t need to be perfect. Just check your meds once a month. Throw out the expired ones. Write down the dates. Set a reminder. That’s it. Over time, this habit keeps your medicine cabinet clean, your health safe, and your money from being wasted on pills you can’t trust. And if you’re helping someone else? You’re not just organizing medicine - you’re protecting their life.

I throw out all my meds every 6 months. No excuses. If it's expired, it's trash. Period.