What Exactly Is Swimmer’s Ear?
Swimmer’s ear isn’t just water stuck in your ear after a dip in the pool. It’s an infection of the outer ear canal-the tube that runs from your eardrum to the outside of your head. When this area gets irritated, moist, or scratched, bacteria or fungi move in and cause inflammation. The result? Pain, itching, swelling, and sometimes even muffled hearing.
It’s called swimmer’s ear because water creates the perfect breeding ground. But you don’t have to be a swimmer to get it. Showering, sweating, or even using cotton swabs can trigger it. The ear canal’s natural defense is its acidic pH, around 5.0 to 5.7. That acidity keeps germs away. But when water washes away earwax or you scratch the skin inside, that protection breaks down.
What Causes Swimmer’s Ear?
The main culprits are two types of germs: Pseudomonas aeruginosa and Staphylococcus aureus. Together, they cause about 60% of cases. Pseudomonas loves wet environments-so pools, hot tubs, and even damp bathrooms are risky. Staph is more common on skin, so scratching your ear with a fingernail or a Q-tip can introduce it.
Fungal infections (otomycosis) are less common but still happen in about 10% of cases. Aspergillus is the usual offender, especially in humid climates. These infections often look different: more itching than pain, with visible white or black fuzz inside the ear.
People with diabetes, eczema, or a weakened immune system are at higher risk. Even a tiny cut in the ear canal can turn into a serious infection in these cases. And if left untreated, it can progress to malignant otitis externa-a rare but dangerous condition that spreads to the skull bone.
How Do You Know It’s Swimmer’s Ear and Not Something Else?
Many people mistake swimmer’s ear for a middle ear infection (otitis media). But the signs are different. With swimmer’s ear, pulling on your earlobe or pressing on the bump in front of your ear (the tragus) makes it hurt. Middle ear infections don’t cause that kind of pain.
Other clues:
- Ear canal looks red and swollen
- Drainage-clear, yellow, or even bloody
- Hearing feels muffled because the canal is blocked
- No fever in mild cases, but high fever means it’s gotten worse
If you’ve had recent water exposure and your ear feels full and tender, it’s likely swimmer’s ear. If you’re unsure, skip the guesswork. A doctor can look inside with an otoscope and tell you for sure.
What Ear Drops Actually Work?
Not all ear drops are created equal. The right one depends on what’s causing the infection-and how bad it is.
For Mild Cases: Acetic Acid + Hydrocortisone
Over-the-counter drops like Swim-Ear (2% acetic acid with hydrocortisone) are a solid first step. They work by restoring the ear’s natural acidity and calming inflammation. Studies show they’re about 85% effective for mild infections. They’re cheap-around $15-and safe for occasional use after swimming to prevent infection.
But here’s the catch: if your ear canal is already swollen shut, these drops won’t reach the infection. They’re for prevention or early-stage cases only.
For Moderate to Severe Cases: Ciprodex (Ciprofloxacin + Dexamethasone)
This prescription combo is the gold standard. Ciprofloxacin kills bacteria, especially Pseudomonas. Dexamethasone reduces swelling and pain. Clinical trials show 92% of people feel better within 7 days. It’s the most commonly prescribed drop in the U.S.
But it’s expensive-around $147.50 without insurance. Some people switch to generic ofloxacin (about $45), which works almost as well but doesn’t include the steroid. That means more pain and slower recovery.
For Fungal Infections: Clotrimazole
If your ear itches like crazy and you see fuzzy stuff inside, it’s probably fungal. Acetic acid won’t help here. Clotrimazole 1% solution works in 93% of cases. You can get it by prescription or sometimes over-the-counter in some countries.
What to Avoid: Neomycin and Other Aminoglycosides
Older drops like neomycin-polymyxin are still sold, but they’re risky. If you have a perforated eardrum (even a tiny one), these can damage your hearing. The FDA warns about this. They’re also more likely to cause allergic reactions-up to 7% of users get contact dermatitis.
How to Use Ear Drops Correctly (So They Actually Work)
Even the best drops fail if you use them wrong. Here’s how to do it right:
- Wash your hands.
- Warm the bottle in your hands for 1-2 minutes. Cold drops can make you dizzy.
- Lie on your side with the infected ear facing up.
- Put in the exact number of drops your doctor or label says.
- Stay still for 5 minutes. Gently tug your earlobe to help the drops go deeper.
- Wipe away any excess that drips out.
- Don’t put cotton swabs, fingers, or anything else in your ear.
Studies show 32% of people skip the 5-minute wait. That cuts effectiveness by 40%. You’re not just putting drops in-you’re letting them soak in.
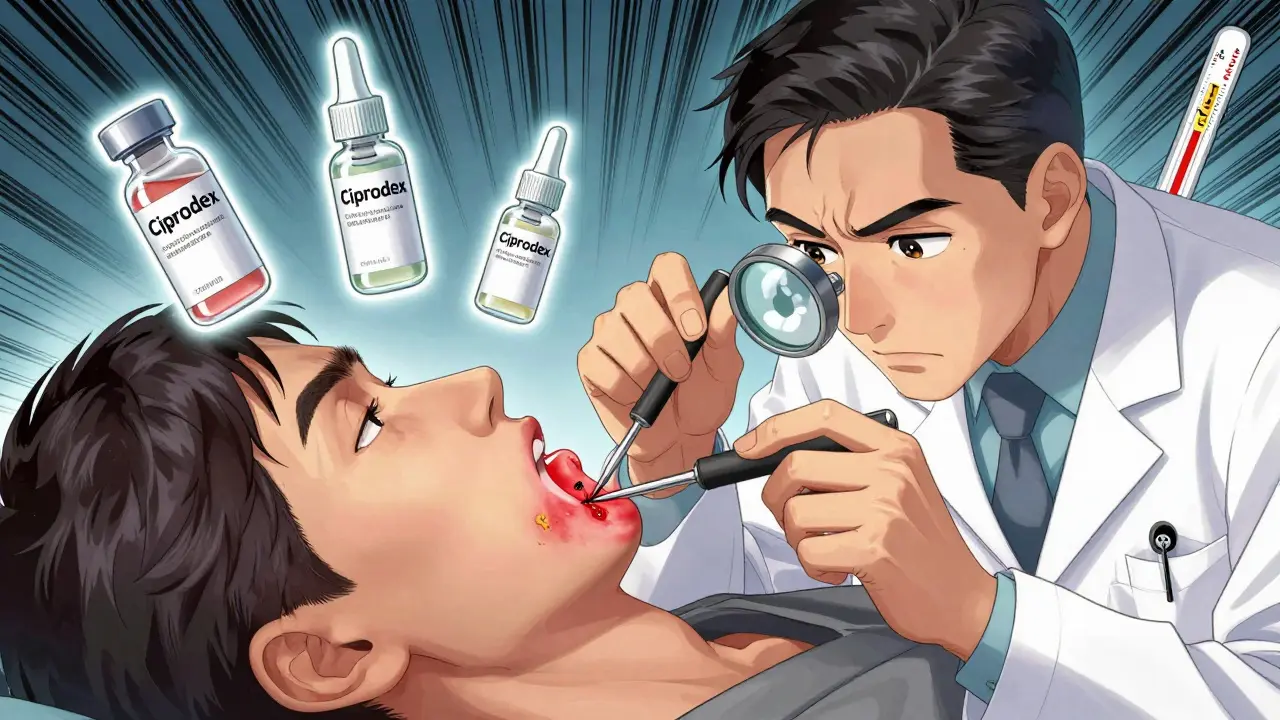
Why Debridement Matters (And Why Most People Skip It)
Doctors often clean out the ear canal before prescribing drops. That’s called debridement. It means removing debris, wax, and pus so the medication can reach the infected skin.
It’s not glamorous. It’s done with a suction tool or a tiny cotton swab under a magnifying scope. But it’s critical. Research shows debridement improves drop effectiveness by 30-40%. If your ear is completely blocked, your doctor might insert a small sponge-like wick to help the drops get through. It’s uncomfortable-but it works.
Most people skip this step because they don’t know to ask for it. If you’ve been using drops for 2-3 days and nothing’s changed, go back. You might need cleaning.
When to See a Doctor
You can try OTC drops for mild symptoms for 2 days. But if any of these happen, see a professional:
- Pain gets worse after 48 hours
- Fever over 101°F (38.3°C)
- Swelling spreads to your neck or face
- You have diabetes or a weakened immune system
- Hearing doesn’t improve after 3 days
Diabetics are at higher risk for complications. Even a small ear infection can turn dangerous fast. Don’t wait.
Preventing Swimmer’s Ear
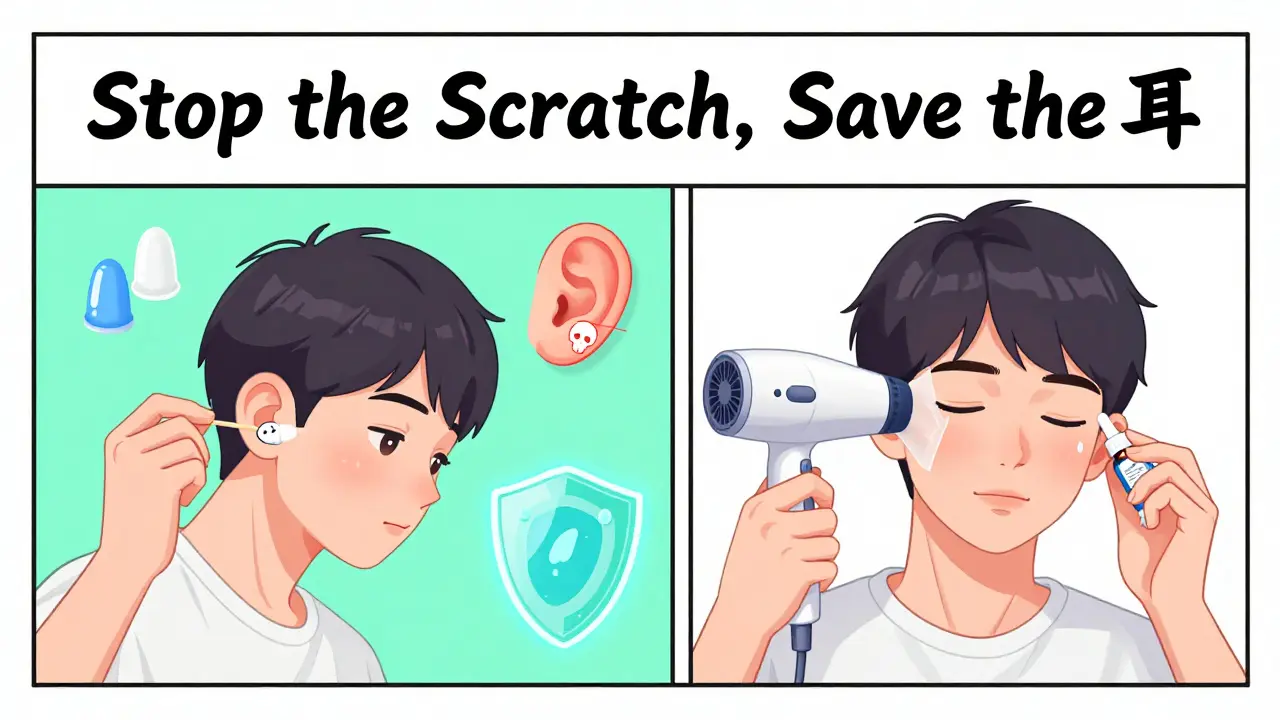
Prevention is easier than treatment. Here’s what works:
- After swimming or showering, tilt your head to drain water.
- Use a hair dryer on low, cool setting, held at arm’s length, to gently dry your ears.
- Use acetic acid drops (like Swim-Ear) after swimming-this cuts recurrence by 65%.
- Avoid cotton swabs. Ever. They push wax deeper and scratch the skin.
- If you swim often, consider custom earplugs. Regular ones can trap water.
People who use preventive drops after swimming report far fewer infections. It’s not magic-it’s just maintaining that protective acidic layer.
What’s New in Treatment?
There’s a new prescription drop called OtiRx, approved in March 2023. It’s a longer-lasting version of ofloxacin, so you only need to use it once a day instead of twice. Early results show 94% effectiveness.
Researchers are also testing microbiome treatments-like probiotic ear drops that restore good bacteria. These are still in trials, but they could change how we think about ear infections in the future.
Common Mistakes That Make Swimmer’s Ear Worse
Based on thousands of patient reports:
- Using hydrogen peroxide or vinegar straight from the bottle-too strong, burns the skin.
- Ignoring fungal infections and using bacterial drops-makes itching worse.
- Stopping drops early because pain is gone-germs can still be there.
- Sharing ear drops-spreads infection.
- Trying to clean the ear canal yourself-leads to more damage.
The biggest mistake? Self-diagnosing. If your ear hurts and you’re not sure, get it checked. Misdiagnosis delays treatment by 7-10 days in about 15% of cases.
Final Thoughts
Swimmer’s ear is common, painful, and easy to treat-if you catch it early and use the right drops. Don’t waste money on ineffective OTC products if your symptoms are moderate or worse. Don’t ignore it because it’s "just an ear infection." And don’t let fear of cost stop you from seeing a doctor. Generic options exist. Preventive drops are cheap. The right treatment gets you back to swimming, showering, and sleeping without pain-in days, not weeks.
