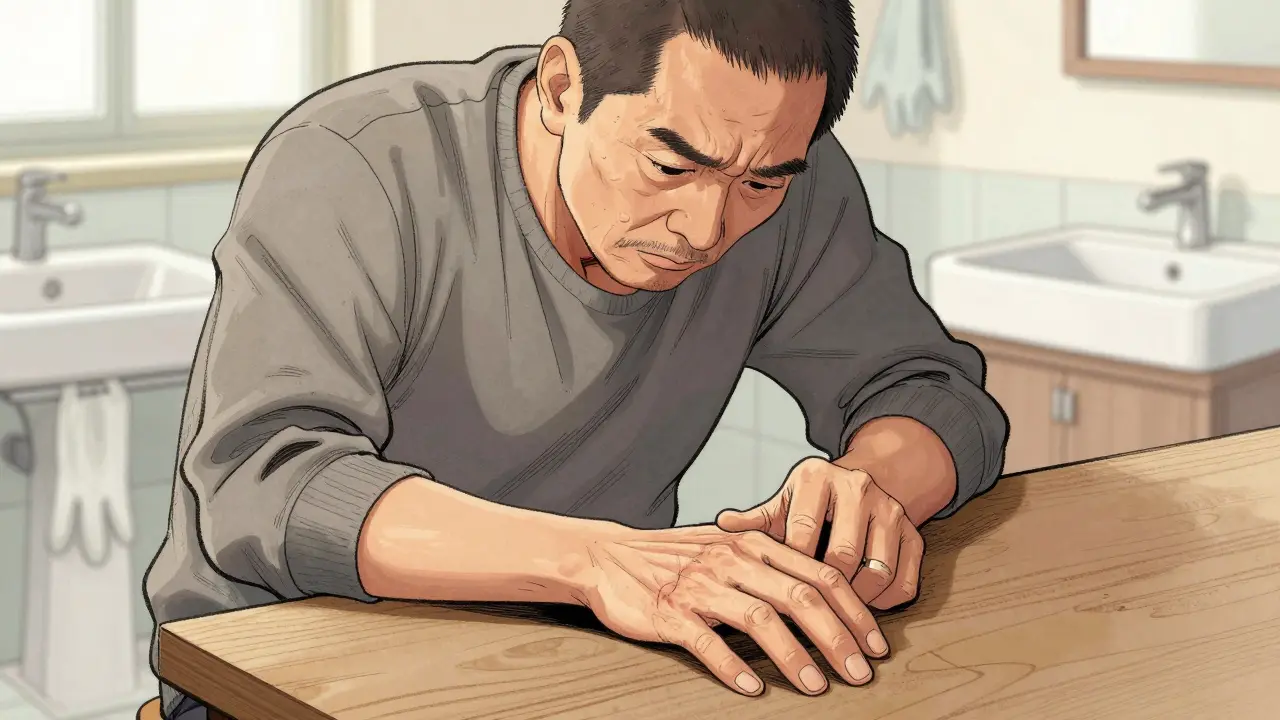
Imagine trying to shake someone’s hand, but your fingers won’t straighten. Or washing your face, and you can’t get your palm flat against your skin. For people with Dupuytren’s contracture, these everyday actions become difficult-or impossible-without intervention. It’s not just a lump in the palm. It’s a slow, silent takeover of hand function, driven by thickening tissue that pulls fingers inward like a tightening rope.
What Exactly Is Dupuytren’s Contracture?
Dupuytren’s contracture starts with a small, painless nodule in the palm, usually near the base of the ring or little finger. Over time, that nodule turns into a tough cord beneath the skin. These cords are made of abnormal collagen and myofibroblasts-cells that behave like tiny muscles, constantly pulling. As they contract, they drag the fingers down toward the palm. The ring finger is affected in over 60% of cases, followed by the little finger. It’s rare for the thumb or index finger to be involved.
This isn’t just a cosmetic issue. When the metacarpophalangeal joint (the knuckle) bends more than 30 degrees, or the proximal interphalangeal joint (the middle knuckle) bends more than 20 degrees, it’s considered clinically significant. At that point, daily tasks get harder: putting on gloves, holding a steering wheel, even resting your hands on a table. The Dupuytren’s contracture doesn’t hurt most of the time, but the loss of function is what drives people to seek help.
Who Gets It-and Why?
Dupuytren’s isn’t random. It runs in families. If you have a parent or sibling with it, your risk jumps to nearly 70%. People of Northern European descent-especially those with Scandinavian or Celtic roots-are far more likely to develop it. In the U.S. and Europe, about 3-6% of adults have it, but among those over 65 with that ancestry, rates climb to 30% or higher.
Genetics play a big role. Studies have found 11 gene locations linked to the condition, with two on chromosomes 16 and 20 explaining about a quarter of inherited risk. It’s also more common in men than women, and it tends to show up earlier and progress faster in men. Other risk factors include diabetes, smoking, heavy alcohol use, and manual labor, but none of these cause it alone. It’s mostly a genetic condition that gets triggered by age and lifestyle.
It often affects both hands, but rarely equally. One hand might have a 45-degree contracture while the other is barely noticeable. That asymmetry is normal. And while it’s slow for most-taking 5 to 15 years to become problematic-some people see rapid changes within a year or two.
How Is It Diagnosed?
Doctors don’t need fancy scans. A simple physical exam is enough. The table top test is the gold standard: if you can’t lay your palm flat on a table, you likely have Dupuytren’s. That’s because the cords prevent full extension. Your doctor will also measure how far your fingers bend using a goniometer, a small tool that measures joint angles.
Early signs include dimpling or puckering of the skin in the palm, which happens as the cords pull underneath. Some people feel a tightness or thickening before they see a visible deformity. If you notice your fingers aren’t straightening like they used to, or your palm feels like it’s got a hard knot, don’t ignore it. Tracking progress at home is easy: use a free app like Hand Meter, which studies show is 95% as accurate as a clinic measurement.

Treatment Options: What Actually Works?
There’s no cure. But there are ways to restore function. Treatment isn’t about removing the disease-it’s about releasing the cords so your fingers can move again. The choice depends on how bad the contracture is, your age, your job, and your tolerance for recovery time.
Needle Aponeurotomy
This is a quick, minimally invasive procedure done in the doctor’s office under local anesthesia. A needle is inserted through the skin and used to cut the cord. It takes about 15 minutes. Most people can move their fingers right away. Success rates for early-stage cases are 80-90%. The big downside? Recurrence. About half of people see the cord come back within three years. But it’s cheap-$1,500 to $3,000-and you’re back to work in days. It’s ideal for older patients or those who can’t handle surgery.
Collagenase Injection (Xiaflex)
Xiaflex is a enzyme that eats collagen. It’s injected directly into the cord. After 24 hours, the doctor manually breaks the cord by straightening the finger. It’s effective for metacarpophalangeal joints, with 65-78% success. But it’s expensive: $3,500 to $5,000 per injection. You need to follow strict post-injection steps: straightening exercises multiple times a day. If you skip them, success drops from 85% to 65%. Side effects include swelling, bruising, and occasionally tendon rupture. It’s not for everyone, but it’s a good middle ground between needle aponeurotomy and surgery.
Open Fasciectomy
This is the traditional surgery: cutting out the diseased tissue. It’s done under general or regional anesthesia. Recovery takes 6-12 weeks. You’ll need physical therapy, splinting, and daily stretching. But it’s the most durable option: only 20-30% of patients see recurrence after five years. The catch? Complications happen in 15-25% of cases-nerve damage, infection, stiffness. It’s the go-to for younger, active people with severe contracture or those who’ve had failed non-surgical treatments.
Dermofasciectomy
This is a more aggressive version of fasciectomy. Not only is the cord removed, but the overlying skin is taken out too and replaced with a skin graft. It reduces recurrence to just 10-15% at five years. But recovery is longer-up to six months-and scarring is more noticeable. It’s reserved for people with very aggressive disease or multiple recurrences.
What Doesn’t Work
Many people try splints, stretches, or special gloves. While gentle stretching can help maintain motion after treatment, there’s no proof that splints or gloves stop progression. A 2023 survey of over 1,500 patients found 28% reported skin breakdown from constant stretching, and 70% saw no improvement after six months of use. Corticosteroid injections were once popular for painful nodules, but studies show they only help 30% of patients and can thin the skin over time. They’re not recommended as a primary treatment anymore.
What About New Treatments?
Research is moving fast. A new device called the Fasciotome, cleared by the FDA in March 2023, uses ultrasound guidance to cut cords with a tiny blade through a needle. It takes just 12 minutes instead of 30. Early results show similar success to needle aponeurotomy but with less bruising.
Gene therapy is on the horizon. A Phase I trial targeting the TGF-β1 protein (which drives collagen overproduction) showed a 40% reduction in cord thickness after six months. And stem cell therapies using fat-derived cells are entering Phase III trials by late 2025. These won’t be available for years, but they represent a shift from managing symptoms to potentially stopping the disease at its source.

Recovery and Real-Life Impact
Success isn’t just about straightening fingers-it’s about keeping them that way. Physical therapy is critical. Patients who did more than 80% of their prescribed exercises regained 95% of their motion. Those who skipped sessions? Only 75%. Home stretching takes discipline: 5-10 minutes, 4-6 times a day. Most people stick with it for three months, then slip back. That’s why follow-up care matters.
For many, the emotional toll is as heavy as the physical. A 2023 survey of 1,247 patients found 89% couldn’t grip things properly, 76% struggled with hygiene, and 68% had job limitations. Manual laborers were over three times more likely to lose work capacity than office workers. One Reddit user, a guitarist, said he got his fingers back in 48 hours after needle aponeurotomy and could play again. Another, with a 60-degree contracture, said Xiaflex gave him 70% improvement but intense pain during the procedure.
When to Act
Not everyone needs treatment. A 2022 study showed 40% of people with less than 30 degrees of contracture never progressed to functional loss over ten years. That’s why many experts recommend a watchful waiting approach until the contracture interferes with daily life. If you can still put your hand flat on a table, you might not need anything yet. But if you can’t, it’s time to talk to a hand specialist.
There’s no rush. Dupuytren’s doesn’t spread like cancer. But once fingers are locked, it’s harder to get them back. The key is catching it early enough to preserve function, but not so early that you’re treating something that might never get worse.
What’s Next?
If you’re noticing changes in your palm or fingers, don’t wait for it to get bad. See a hand specialist. Bring your phone with the Hand Meter app to track your progress. Ask about your options-not just what’s available, but what’s right for you. Consider your age, your job, your tolerance for recovery, and your risk of recurrence.
Dupuytren’s contracture isn’t life-threatening. But it can steal your independence. The good news? We have more tools now than ever to help you keep your hands working-for shaking, for gripping, for living.
Can Dupuytren’s contracture go away on its own?
No, Dupuytren’s contracture doesn’t reverse itself. The cords that pull the fingers down are made of permanent scar-like tissue. Without treatment, they only get tighter over time. Some people have slow progression and never need intervention, but the condition won’t disappear without medical help.
Is Dupuytren’s contracture painful?
Usually not. Most people notice a painless nodule or thickening in the palm. Pain is rare unless the nodule is new and inflamed, or if you’ve had an injection or surgery. The main issue isn’t pain-it’s losing the ability to use your hand normally.
Can I prevent Dupuytren’s contracture?
Not if you have the genes. But avoiding smoking, limiting alcohol, and managing diabetes may help slow progression. There’s no proven way to stop it from starting, but staying healthy can reduce how fast it worsens.
How do I know if I need surgery?
If you can’t lay your palm flat on a table (positive table top test) and your fingers are bent more than 30 degrees at the knuckle or 20 degrees at the middle joint, it’s time to consider treatment. Your doctor will also look at how much it’s affecting your daily life-gripping, washing, working-before recommending surgery.
What’s the recurrence rate after treatment?
It varies by treatment. Needle aponeurotomy has a 30-50% recurrence rate within three years. Collagenase is around 40% at five years. Open fasciectomy has a 20-30% recurrence rate at five years. Dermofasciectomy drops that to 10-15%. Recurrence doesn’t mean failure-it just means the condition can return, and you might need another procedure later.
Are there any home remedies that help?
Stretching and splinting can help maintain flexibility after treatment, but they don’t stop the disease from progressing. Special gloves or creams won’t cure it. The only proven home tool is tracking your progress with a goniometer app like Hand Meter. It helps you know when it’s time to see a doctor.
Can Dupuytren’s affect other parts of the body?
Yes, in some cases. People with Dupuytren’s are more likely to develop similar conditions in the feet (Ledderhose disease) or the penis (Peyronie’s disease). These are all fibroproliferative disorders linked to the same genetic factors. If you have one, your doctor may check for the others.
How long does recovery take after surgery?
It depends on the surgery. Needle aponeurotomy: you’re back to light activity in 1-2 days. Collagenase: 1-2 weeks with stretching. Open fasciectomy: 6-12 weeks of therapy and splinting. Dermofasciectomy: 3-6 months. Full recovery means regaining motion, strength, and confidence in using your hand.
Hey everyone-just wanted to say how much I appreciate this breakdown. I’ve seen this condition in my dad, and it’s scary how quietly it creeps in. The fact that we now have options like needle aponeurotomy and Xiaflex gives me real hope. It’s not just about function-it’s about keeping the little things: shaking hands, hugging, holding a coffee cup without thinking about it. You’re not alone if you’re dealing with this.