What Is Intrahepatic Cholestasis of Pregnancy?
Imagine waking up in your third trimester with unbearable itching-no rash, no bug bites, just relentless, skin-deep itch that gets worse at night. If you’ve experienced this, you might be dealing with intrahepatic cholestasis of pregnancy (ICP), a liver condition that only happens during pregnancy. It’s not caused by anything you did or didn’t do. It’s a biological glitch triggered by pregnancy hormones, especially estrogen, in women who are genetically prone to it.
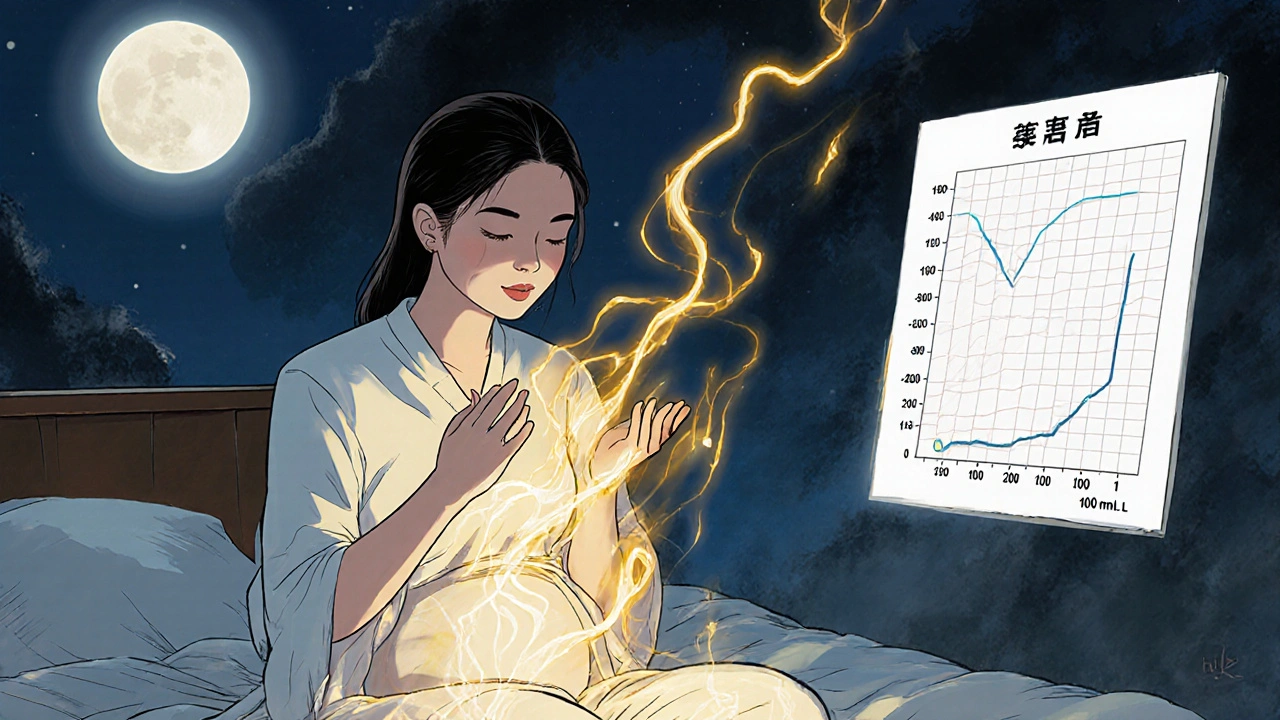
ICP disrupts how your liver moves bile out of your body. Normally, bile helps digest fats and gets flushed out through your intestines. But with ICP, bile acids build up in your bloodstream instead. That’s what causes the itching. The higher the bile acid levels, the greater the risk to your baby. Levels above 10 µmol/L confirm the diagnosis, and anything over 100 µmol/L is considered severe, with stillbirth risk jumping from less than 0.3% to over 3%.
Who Gets ICP-and Why?
ICP doesn’t affect everyone equally. In the U.S., it happens in about 1 to 2 out of every 1,000 pregnancies. But if you’re of Latina descent, especially from Chile or Bolivia, your risk jumps to nearly 6%. In some parts of South America, it’s as common as 1 in 7 pregnancies. Family history matters too-if your mom or sister had ICP, you’re 12 to 15 times more likely to get it.
Other risk factors include carrying twins or triplets, which triples your chance, or having had ICP in a previous pregnancy (up to 70% recurrence). Even IVF pregnancies carry double the risk. It’s not about being overweight or eating poorly-it’s genetics and hormones working together in ways we’re still learning about.
How Is ICP Diagnosed?
There’s no single symptom that screams ICP. The main one is intense itching, usually on the palms and soles, but it can spread. No rash. No redness. Just itching that makes you want to scratch your skin off. Many women are misdiagnosed with dry skin or allergies first.
Doctors confirm ICP with a blood test for serum bile acids. That’s the gold standard. Liver enzymes like ALT and AST may also be elevated, but they’re not reliable on their own. A new tool called autotaxin is showing up in research-it’s 98% accurate at spotting ICP, but not yet widely available.
And here’s the catch: bile acid levels can spike fast. One study found that 30% of women with mild ICP go from safe to dangerous levels in just two weeks. That’s why repeat testing every 1-2 weeks is non-negotiable.
Why Is ICP Dangerous for the Baby?
ICP is mostly uncomfortable for moms-but it’s serious for babies. High bile acid levels can trigger premature labor, fetal distress, or stillbirth. About 30-60% of women with ICP deliver early, depending on how high their bile acids climb. Stillbirth risk rises sharply above 100 µmol/L, which is why doctors don’t wait until 40 weeks.
Unlike other pregnancy liver problems like HELLP or AFLP, ICP doesn’t cause high blood pressure, liver failure, or bleeding. But its silent threat to the baby is why it’s taken so seriously. That’s why monitoring starts early: twice-weekly non-stress tests from 32 weeks, and sometimes daily fetal kick counts at home.

What Treatments Are Safe During Pregnancy?
The only FDA-approved medication for ICP is ursodeoxycholic acid (UDCA). It’s taken as a pill, usually 10-15 mg per kilogram of body weight daily. For a 70 kg woman, that’s about 700-1,050 mg per day. UDCA reduces itching by 70% in most cases and may lower the risk of preterm birth by up to 25%.
But here’s the debate: while UDCA helps with symptoms, a major 2022 Cochrane Review found no clear proof it reduces stillbirths. That doesn’t mean it doesn’t help-it just means we don’t have big enough studies yet to be 100% sure. Still, most doctors prescribe it because the benefits outweigh the risks. It’s safe for mom and baby, with almost no side effects.
Other options exist, but they’re second-line. S-adenosyl methionine (SAMe) can ease itching for some women, but there’s limited data. Cholestyramine (a bile acid binder) helps some, but it can block vitamin K absorption-raising the risk of postpartum bleeding. That’s why it’s used sparingly.
When Should You Deliver?
Delivery timing is the biggest decision in ICP care. If your bile acids are under 40 µmol/L, most experts recommend delivery at 37-38 weeks. If they’re above 100 µmol/L, delivery may happen as early as 34-36 weeks. Some centers now use a personalized approach: tracking bile acid trends over time instead of relying on one number.
A new 2024 guideline, still in draft, suggests that with close monitoring and UDCA, stillbirth risk stays below 0.5% even at 38 weeks-even if bile acids are mildly elevated. That could mean fewer unnecessary early deliveries. But in places without regular testing, doctors still rely on symptoms alone, which increases risk.
What Happens After Baby Is Born?
Good news: ICP disappears within days after delivery. Liver enzymes and bile acids return to normal. No long-term liver damage. You won’t need ongoing treatment.
But here’s something many women don’t know: having ICP raises your risk for liver problems later in life. Studies show you’re 3.2 times more likely to develop gallstones, chronic hepatitis, or even hepatitis C decades later. That doesn’t mean you will-but it means you should tell your future doctors about your ICP history. Get routine liver checks after your 40s, especially if you have other risk factors like obesity or alcohol use.
What’s New in ICP Care?
Technology is catching up. In 2023, the FDA approved a new point-of-care test called CholCheck®. It gives bile acid results in 15 minutes instead of waiting days. It’s already in use at 65% of high-risk maternity hospitals in the U.S.
Researchers are also testing new drugs called autotaxin inhibitors. Early trials show they cut itching by nearly 70% in just four weeks. These could be game-changers-if they pass safety testing for pregnancy.
But access isn’t equal. In Scandinavia, all pregnant women get routine bile acid screening in the third trimester. In the U.S., only 42% of OB-GYNs test unless symptoms appear. That delay-often 7 to 10 days-means more babies are at risk.
What Should You Do If You Suspect ICP?
- Don’t ignore persistent itching, especially if it’s worse at night or on your hands and feet.
- Ask your doctor for a serum bile acid test-don’t wait for a rash or jaundice.
- If diagnosed, get referred to a maternal-fetal medicine specialist.
- Start UDCA if recommended, and stick with it.
- Do twice-weekly non-stress tests and count kicks daily.
- Know your bile acid numbers and track how they change.
- Prepare for delivery between 34 and 38 weeks, depending on your levels.
- After birth, tell your primary care doctor about your ICP history.
How to Reduce Anxiety With ICP
ICP is scary. The fear of losing your baby is real. But education helps. Women who get clear, detailed info about ICP report 22% less anxiety and stick to treatment 18% better than those who just get a quick explanation.
Ask for printed materials. Watch videos from trusted sources like the American Liver Foundation. Join a support group. You’re not alone. Thousands of women go through this every year-and most deliver healthy babies when they’re monitored closely.
ICP is a textbook example of why we need mandatory bile acid screening at 28 weeks-period. The fact that 42% of OB-GYNs in the U.S. wait for symptoms? That’s not negligence; it’s systemic malpractice. The FDA approved CholCheck® in 2023; it’s not a luxury-it’s a standard of care. If your provider isn’t offering it, demand it. Or switch. Stillbirth risk isn’t a "maybe"-it’s a statistical inevitability when bile acids exceed 100 µmol/L. This isn’t about anxiety; it’s about biochemistry. And if your doctor dismisses itching as "dry skin," they’re not just outdated-they’re dangerous.