Probiotic Safety Checker for Immunosuppressed Patients
How Safe Are Probiotics For You?
This tool helps assess your personal risk of probiotic-related infections based on your medical condition, medications, and device use. Always consult your doctor before taking any supplements.
Medical Condition
Medications & Devices
Probiotic Type
Risk Assessment
When you're on immunosuppressants-whether after a transplant, for an autoimmune disease, or during chemotherapy-your body is already playing defense. Every infection, even a minor one, can turn serious fast. Now add probiotics into the mix. They’re marketed as harmless, even helpful. But for people with weakened immune systems, they can be dangerous. This isn’t theoretical. People have gotten sepsis from probiotics. Some have died.
Why Probiotics Aren’t Always Safe for Immunosuppressed People
Probiotics are live bacteria or yeast. They’re supposed to help your gut. For healthy people, they often do: reducing diarrhea after antibiotics, easing bloating, improving regularity. But in someone whose immune system is turned down by drugs like tacrolimus, mycophenolate, or prednisone, those same microbes can slip through the gut lining and enter the bloodstream. Once there, they find a quiet, nutrient-rich place with no immune soldiers to stop them. That’s how a daily probiotic pill turns into a hospital stay. The most common culprits? Lactobacillus rhamnosus GG and Saccharomyces boulardii. The yeast, Saccharomyces boulardii, is especially risky. It’s been linked to bloodstream infections in patients with central lines, and in some cases, it’s killed nearly a quarter of those infected. A 2021 review of 47 cases found that 83% of probiotic-related infections happened in people with weakened immune systems. About 36% of those cases were fatal. That’s not a small risk. That’s a life-or-death calculation.Who’s at the Highest Risk?
Not everyone on immunosuppressants is equally at risk. The danger depends on how weak the immune system is, what drugs are being used, and whether there are other medical devices in play.- Neutropenia (absolute neutrophil count below 500 cells/µL): This is the reddest of red flags. If your body can’t make enough white blood cells to fight infection, probiotics are off-limits. Most cancer centers in the U.S. ban them during chemotherapy-induced neutropenia.
- Recent organ transplant: Especially in the first three months. Your body is being flooded with drugs to prevent rejection. That’s when your defenses are at their lowest. Studies show a spike in probiotic-related infections during this window.
- Central venous catheters: If you have a port, PICC line, or central line, Saccharomyces boulardii can cling to it and grow. One study found a 27% higher risk of bloodstream infection when people with catheters took this yeast.
- Stem cell transplant: Bone marrow transplants leave patients vulnerable for months. A 2020 study found these patients were over four times more likely to get a probiotic-related blood infection than those who didn’t take them.
- Low CD4 count in HIV: If your CD4 count is under 100, your risk of fungal infections from probiotics jumps nearly fourfold. Above 200? Risk is low.
Who Might Be Okay? (And What Strains Matter)
This isn’t a blanket no. Some people can use probiotics safely-if they’re careful. Liver transplant patients, for example, showed a 34% drop in bacterial infections in one 2022 study-with no increase in serious side effects. That’s the only group with strong evidence of benefit. Even then, experts recommend using only single-strain products and getting clearance from an infectious disease specialist. The strain matters more than you think. Lactobacillus rhamnosus GG is the most commonly studied and the most commonly linked to infections. But not all Lactobacillus strains are the same. Some are safer than others. The same goes for Bifidobacterium. Most commercial probiotics contain 5 to 10 strains. That’s a problem. More strains mean more chances for something to go wrong. A 2022 study showed that single-strain probiotics had 63% less risk of translocation (leaking into the blood) than multi-strain blends. If you’re in a moderate-risk group, ask your doctor for a product with just one strain, and make sure they know the exact name: Lactobacillus rhamnosus GG ATCC 53103, not just “Lactobacillus.”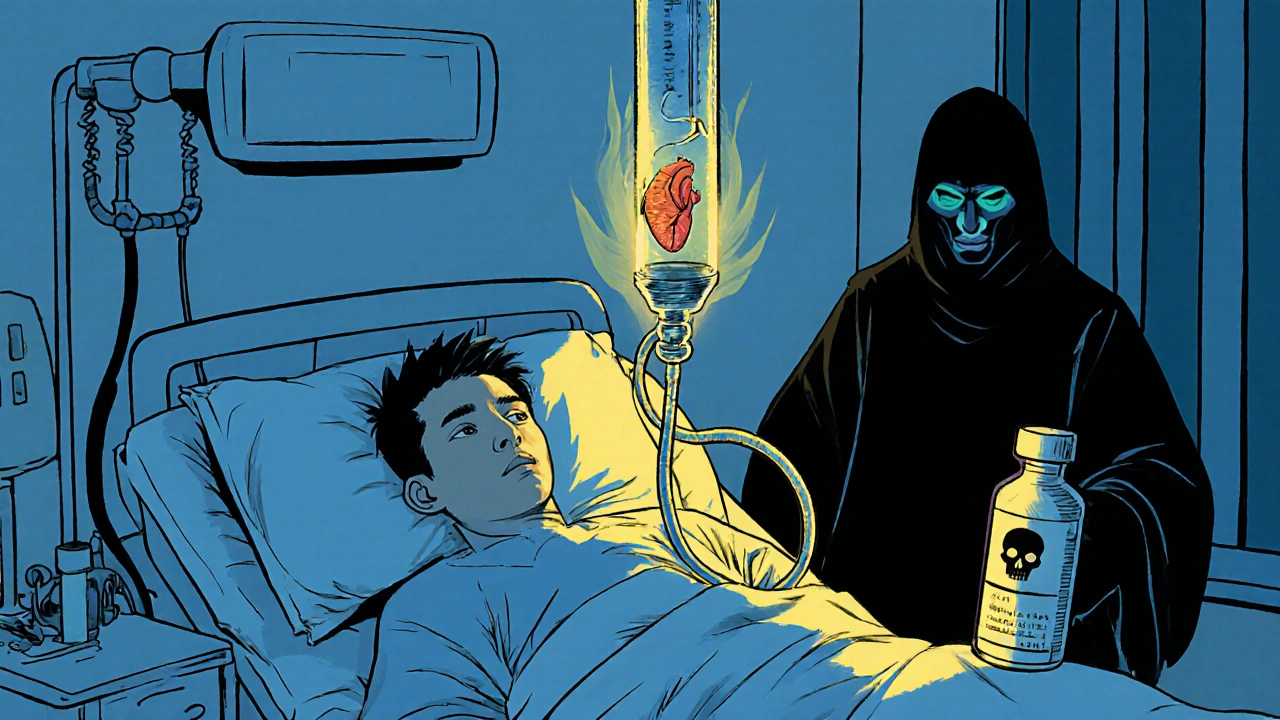
What the Guidelines Say
Medical groups don’t agree on everything, but here’s what the major ones recommend:- Infectious Diseases Society of America (IDSA), 2023: Uses a four-tier risk system. Highest risk? Absolute no. Moderate risk? Only with specialist approval. Low risk? Maybe, if it’s a single strain and you’re stable.
- ESPEN (European Society for Clinical Nutrition): Strongly advises against probiotics in critically ill immunocompromised patients.
- American Gastroenterological Association: Only conditionally recommends specific strains for liver disease patients with hepatic encephalopathy.
- Optibac Probiotics (2023): Explicitly says: “We do not recommend that individuals who are immunosuppressed take live cultures supplements.”
Real Stories, Real Consequences
Case reports tell the real story. One patient, recovering from a kidney transplant, started a probiotic for digestion. Within a week, he developed fever, chills, and sepsis. Blood cultures grew Lactobacillus. He spent 19 days in the ICU. Another, on methotrexate for rheumatoid arthritis, took a Saccharomyces boulardii supplement for three months. She developed fungemia. Her heart was infected. She needed surgery. But not everyone has bad outcomes. Some autoimmune patients report fewer digestive issues without complications. A 2022 survey of 1,247 people found 68% felt better on probiotics. But here’s the catch: they didn’t track immune status. Did they have low neutrophils? Were they on multiple drugs? We don’t know. That’s the problem with anecdotal evidence-it doesn’t control for risk.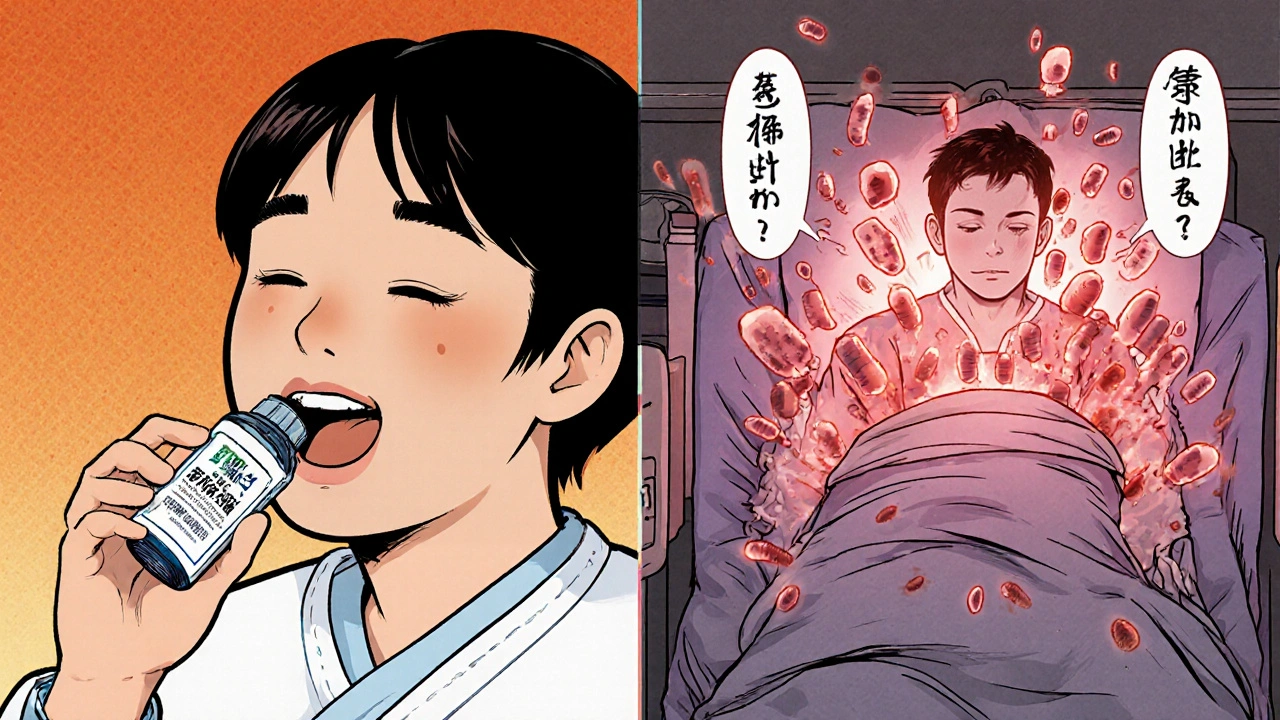
What You Should Do
If you’re on immunosuppressants:- Don’t start probiotics without talking to your doctor. Not your pharmacist. Not your nutritionist. Your prescribing physician or infectious disease specialist.
- If you’re already taking them, stop. Especially if you’ve got a central line, low neutrophils, or are in the first three months post-transplant.
- Ask for strain-specific advice. If your doctor says yes, demand the exact strain name and lot number. Not “Lactobacillus.” Not “a blend.” The exact strain.
- Watch for fever. If you develop a temperature over 38.3°C (101°F), stop the probiotic immediately and get blood cultures. Don’t wait.
- Consider alternatives. Prebiotics (fiber that feeds good bacteria) and postbiotics (inactive microbial parts) are being studied as safer options. One trial showed postbiotics reduced C. diff infections without any infections from the supplement itself.
The Bigger Picture
The probiotic market is worth over $50 billion. Most products are sold as supplements, not drugs. That means they don’t have to prove safety for high-risk groups before hitting shelves. The FDA didn’t require warning labels on Saccharomyces boulardii until July 2023-after 14 cases of fungemia in immunocompromised patients. Hospitals are catching up. In 2023, 62% of U.S. academic medical centers had formal probiotic protocols for immunosuppressed patients. In 2018, it was 28%. Progress is slow, but it’s happening. Right now, the safest choice for anyone on immunosuppressants is to avoid probiotics unless there’s clear, documented benefit and expert oversight. The potential upside-slightly better digestion-isn’t worth the risk of sepsis, heart infection, or death.What’s Next?
A new global registry called PROTECT is tracking 5,000 immunosuppressed patients on probiotics across 47 centers. Results are expected in 2025. Until then, we’re working with what we have: real cases, real deaths, and a growing body of evidence that says: when your immune system is down, treat microbes like strangers-not friends.Can I take probiotics if I’m on prednisone?
It depends. If you’re on low-dose prednisone for a stable condition like asthma or rheumatoid arthritis, and you have no other immune issues, the risk is low-but not zero. If you’re on high doses, have other immunosuppressants, or have a central line, avoid them. Always check with your doctor. Prednisone alone doesn’t always mean danger, but combined with other factors, it can.
Is Saccharomyces boulardii more dangerous than bacterial probiotics?
Yes. Saccharomyces boulardii is a yeast, not a bacterium. In immunocompromised people, it’s more likely to cause bloodstream infections (fungemia) than bacterial strains. It’s also harder to treat. Case fatality rates for Saccharomyces-related infections have reached 22%. It’s also the strain most often linked to infections in patients with central venous catheters. Most experts recommend avoiding it entirely if you’re immunosuppressed.
Are probiotics regulated like drugs?
No. In the U.S., most probiotics are sold as dietary supplements, not medications. That means they don’t need FDA approval before being sold. Manufacturers don’t have to prove they’re safe for people on immunosuppressants. The FDA only stepped in to require warning labels on Saccharomyces boulardii products in 2023 after multiple deaths. Many products still don’t list strain names clearly.
Can I get probiotics from food instead of supplements?
Fermented foods like yogurt, kefir, sauerkraut, and kimchi contain live microbes, but in much smaller amounts than supplements. For most immunosuppressed people, these are considered low risk-unless you’re severely neutropenic or have a central line. Still, avoid unpasteurized products if your immune system is very weak. Pasteurized versions are safer. Always check with your care team.
What are postbiotics, and are they safer?
Postbiotics are non-living microbial components-like cell walls, enzymes, or metabolites-that may support gut health without the risk of infection. Since they’re not alive, they can’t cause sepsis. Early trials show promise: one phase 2 trial reduced C. diff infections in immunosuppressed patients by 40% with zero infections from the product itself. They’re not widely available yet, but they represent the future of safe microbiome support for high-risk patients.
Should I stop probiotics before surgery or a transplant?
Yes. Most transplant centers require patients to stop all probiotics at least two weeks before surgery. The goal is to reduce the chance that gut microbes will enter the bloodstream during the procedure or during the early recovery phase when immunosuppression is highest. Even if you’ve taken them without issue before, your body’s defenses will be lower after transplant. Don’t risk it.

Y'all need to stop popping probiotics like candy! I had a friend on chemo who took them 'for digestion' and ended up in the ICU for weeks. Don't be that person. Your gut ain't worth your life.