Working nights isn’t just inconvenient-it’s physically disruptive. If you’ve ever tried to sleep during the day after a 12-hour shift, only to be woken up by sunlight, kids, or the neighbor’s lawnmower, you’re not lazy. You might have shift work sleep disorder (SWSD). This isn’t just bad sleep habits. It’s a medically recognized circadian rhythm disorder that affects millions of people who work outside the 9-to-5 window.
What Exactly Is Shift Work Sleep Disorder?
SWSD happens when your body’s internal clock-your circadian rhythm-gets completely out of sync with your work schedule. Your brain is wired to be awake during daylight and asleep at night. When you force yourself to be alert from 11 p.m. to 7 a.m. and try to sleep from 8 a.m. to 4 p.m., your body fights back. Melatonin, the sleep hormone, keeps rising when you’re supposed to be working. Cortisol, the wake-up hormone, dips when you need to be alert. The result? Insomnia, extreme fatigue, and brain fog that doesn’t go away.
The American Academy of Sleep Medicine officially recognized SWSD in 2005. Since then, research has shown that 10% to 30% of night and rotating shift workers develop symptoms severe enough to be diagnosed. That’s up to 4 million Americans alone who are struggling with this disorder every single day.
Why Your Body Won’t Adapt (Even After Years)
Many people think, “I’ve been working nights for five years-I should be used to it by now.” But science says otherwise. Studies from Brigham and Women’s Hospital show that only 2% to 5% of night shift workers ever fully adapt their circadian rhythms. Even after decades, most people’s bodies still think it’s nighttime when they’re awake-and daytime when they’re trying to sleep.
Why? Because light is the strongest signal your brain uses to reset its clock. Artificial light at night-especially blue light from screens and fluorescent bulbs-tricks your brain into thinking it’s still daytime. That suppresses melatonin by up to 85%. Meanwhile, sunlight streaming through your blinds during the day tells your brain to wake up, even when you’re exhausted.
It’s not just about willpower. Your genes play a role too. People with a “night owl” chronotype adapt 37% better than “morning larks.” If you’ve always been a late sleeper, you’re more likely to handle nights. But if you naturally wake up at 6 a.m., your body is fighting an uphill battle.
What Does SWSD Actually Feel Like?
It’s not just “being tired.” SWSD causes real, measurable problems:
- Struggling to fall asleep or stay asleep during the day-even with blackout curtains, earplugs, and white noise
- Feeling groggy, slow, or confused during your shift
- Dozing off unexpectedly-during meetings, while driving, or even while operating machinery
- Memory lapses, trouble focusing, or making mistakes you wouldn’t normally make
- Mood swings, irritability, or feeling depressed
- Digestive issues, headaches, or weakened immunity
A 2022 Healthline survey found that 78% of shift workers reported excessive sleepiness during work hours. Nearly half said they’d made a mistake at work because of fatigue. One nurse on Reddit described working ER night shifts and only getting 4 hours of sleep-despite every trick in the book. That’s not normal. That’s SWSD.
The Hidden Costs: Safety, Health, and Relationships
SWSD doesn’t just hurt your sleep-it hurts your life.
Workers with untreated SWSD are 2 to 3 times more likely to have workplace accidents. A 2021 case study documented a $2.3 million equipment failure at a Midwest factory caused by a fatigued worker. The National Safety Council estimates fatigue-related errors cost U.S. businesses $13 billion a year.
Long-term health risks are even worse. The International Agency for Research on Cancer classifies shift work as “probably carcinogenic.” Studies link chronic night work to higher risks of breast cancer, colorectal cancer, heart disease, and type 2 diabetes. Why? Because disrupted sleep messes with your immune system, hormone balance, and metabolism.
Relationships suffer too. Missing family dinners, birthdays, and school events becomes normal. Partners get frustrated. Kids don’t understand why Mom or Dad is always asleep. One survey found 63% of shift workers reported strain in their personal relationships because of their schedule.
What Actually Works: Evidence-Based Strategies
There’s no magic fix-but there are proven ways to manage SWSD. The American Academy of Sleep Medicine recommends these three core strategies:
1. Light Therapy: Control Your Environment
Use bright light (10,000 lux) during your night shift. Wear light therapy glasses or sit near a 10,000-lux light box for 30 to 60 minutes every 2 hours. This tells your brain it’s daytime, boosting alertness and suppressing melatonin when you need to be awake.
On your way home, wear blue-light-blocking glasses (amber or red lenses). They help your body start producing melatonin sooner. A 2022 study showed 57% of shift workers who used this combo reported improved alertness and sleep quality.
2. Melatonin Supplementation
Take 0.5 to 5 mg of melatonin 30 minutes before your daytime sleep. Don’t take it during your shift-it’ll make you sleepy when you need to be awake. Melatonin helps shift your internal clock over time. Studies show it can improve sleep duration by 30 to 60 minutes per night.
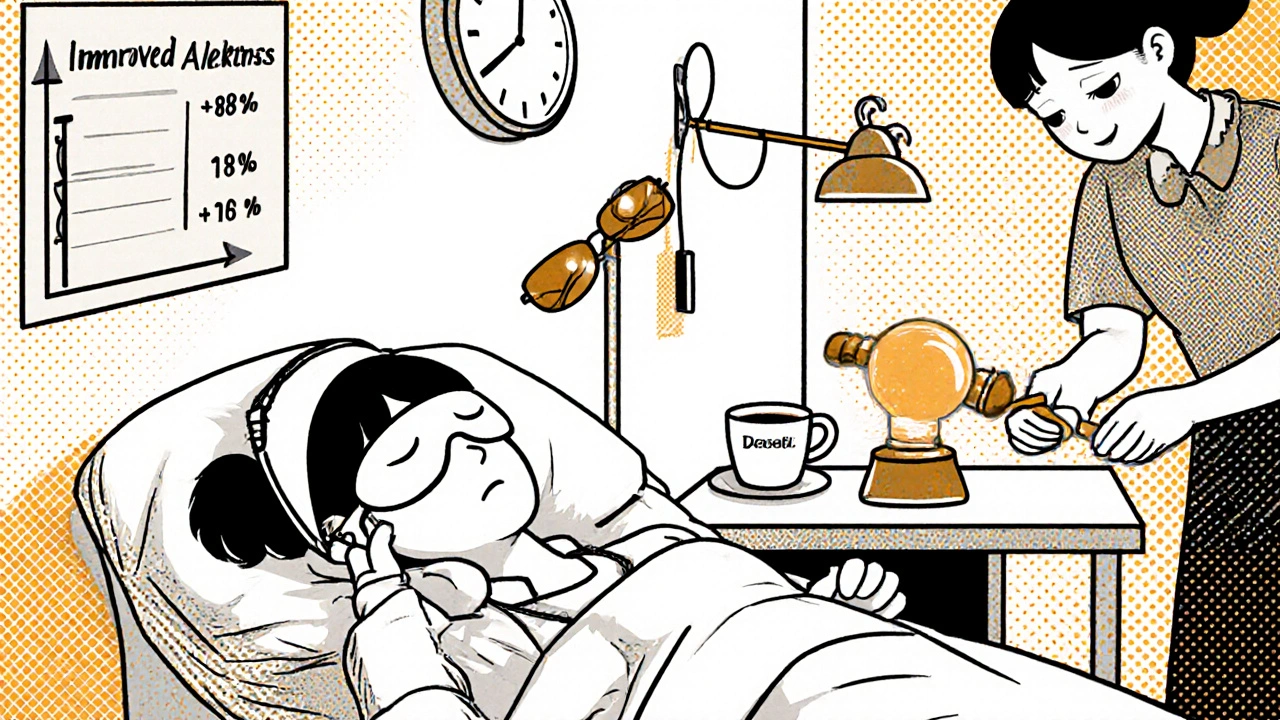
3. Strategic Caffeine Use
Caffeine can help-but timing matters. Have your last cup no later than 2 hours before your planned sleep. Too much too late will wreck your sleep. Stick to 200 mg per dose (about one strong coffee). Avoid energy drinks-they cause crashes and disrupt sleep longer.
4. Naps Are Your Secret Weapon
A 20- to 30-minute nap before your shift can boost alertness by 40%. If your workplace allows it, take a nap during a break. Nurses in one study reported 68% improvement in alertness after using pre-shift naps. Don’t nap longer than 30 minutes-it can leave you groggy.
5. Sleep Hygiene for Daytime Sleep
Your bedroom needs to be a cave:
- Blackout curtains or a sleep mask
- White noise machine or earplugs
- Keep the room cool (65°F or lower)
- Never use your bed for anything but sleep
- Set a consistent sleep schedule-even on days off
Consistency is key. Even on your day off, try to sleep at the same time. Changing your schedule by more than 2 hours throws your rhythm off again.
What Doesn’t Work (And Why)
Many people try quick fixes that don’t help-or make things worse:
- Alcohol to fall asleep: It makes sleep shallow and disrupts REM cycles. You’ll wake up more tired.
- Sleeping pills: They don’t fix circadian misalignment. They just sedate you. Long-term use leads to dependence and worse sleep quality.
- “Just sleep more on days off”: Trying to catch up on sleep doesn’t reverse the damage. Your body can’t reset in one day.
- Ignoring symptoms: Thinking it’s “just part of the job” leads to burnout, health decline, and accidents.
When to See a Doctor
If you’ve had symptoms for more than a month-especially if they’re affecting your work, health, or relationships-it’s time to see a sleep specialist. Diagnosis usually involves:
- A sleep diary tracked for 14 days
- Actigraphy (a wrist device that tracks movement and light exposure)
- Rule out other sleep disorders like sleep apnea or restless legs
Doctors may prescribe FDA-approved medications like modafinil or armodafinil for excessive sleepiness. In May 2023, the FDA approved sodium oxybate specifically for SWSD-a major step forward.
Employers Have a Role Too
SWSD isn’t just an individual problem-it’s an organizational one. Only 22% of shift workers have access to quiet, dark sleeping facilities at work, even though NIOSH recommends them. Companies that invest in SWSD management save money:
- For every $1 spent on light therapy, naps, or scheduling changes, companies save $5.20 in reduced errors and absenteeism.
- Forty-seven percent of U.S. hospitals now screen for SWSD-up from 12% in 2018.
- The EU limits consecutive night shifts to four. The U.S. has no federal limits-but some states are starting to follow.
If your employer doesn’t offer support, ask for it. Bring data. Suggest simple changes: better lighting on shifts, scheduled nap breaks, or access to light therapy devices.
The Future: Personalized Sleep Science
Researchers are now looking at genetics. Some people have variations in the PER3 and CLOCK genes that make them more or less resilient to shift work. Clinical trials are testing personalized treatments based on DNA.
Wearable tech is also advancing. By 2025, 68% of major healthcare systems plan to use devices that track circadian rhythms in real time-giving workers personalized sleep advice based on their body’s actual response.
But here’s the hard truth: human biology isn’t built for permanent night shifts. Dr. Till Roenneberg’s research shows only 1% to 2% of people can adapt fully-even after decades. That’s why the goal isn’t to “get used to it.” It’s to manage it as well as possible, protect your health, and push for better workplace policies.
Final Thoughts: You’re Not Alone
Working nights is tough. Your body isn’t broken-you’re just working against your biology. The good news? You can take control. Use light, melatonin, naps, and strict sleep routines. Talk to your doctor. Advocate for better conditions at work. And remember: this isn’t something you have to suffer through. There are real, science-backed ways to protect your sleep, your health, and your life.
Can you fully adapt to night shifts?
Only 2% to 5% of night shift workers ever fully adapt their circadian rhythms, even after years on the schedule. Most people’s bodies never fully reset, which is why SWSD is a chronic condition for many. The goal isn’t to become a night person-it’s to manage the misalignment with smart strategies.
How long does it take to see improvement with SWSD treatments?
Most people notice improvements in sleep and alertness within 2 to 4 weeks of consistently using light therapy, melatonin, and naps. But it takes ongoing discipline-missing even a few days can throw your rhythm off again.
Is melatonin safe for long-term use in shift workers?
Yes, melatonin is generally safe for long-term use at low doses (0.5-5 mg). It’s a natural hormone your body already produces. Studies show no serious side effects when used correctly. Avoid high doses-they can cause drowsiness, headaches, or nausea. Always take it 30 minutes before daytime sleep, not during your shift.
Do blackout curtains really help daytime sleep?
Yes-especially if paired with white noise and a cool room. Sunlight is the strongest signal that tells your brain to wake up. Even small amounts of light leaking in can prevent deep sleep. Heavy blackout curtains or a sleep mask can increase total sleep time by 30 to 60 minutes per night.
Can SWSD lead to permanent health damage?
Yes. Long-term shift work is linked to higher risks of heart disease, diabetes, obesity, depression, and certain cancers. The body’s inability to repair itself during disrupted sleep cycles is the main reason. The earlier you manage SWSD, the lower your long-term health risks.
Are there any new medications for SWSD?
In May 2023, the FDA approved sodium oxybate specifically for excessive sleepiness caused by SWSD. It’s the first drug approved for this exact use. Modafinil and armodafinil have been used for years, but sodium oxybate offers a new option with a different mechanism of action. Always use these under medical supervision.

It’s not about willpower. It’s about biology. We were never meant to outsmart the sun.
Just saying.