Carbamazepine Drug Interaction Calculator
Carbamazepine is a strong CYP3A4 and CYP2B6 inducer that can reduce exposure to many co-administered drugs by 30-80%. Use this tool to calculate appropriate dose adjustments.
Enter values above to see dose adjustment results.
When prescribing Carbamazepine is a broad‑spectrum anticonvulsant and mood stabilizer, clinicians must keep an eye on its power to turn on the body’s drug‑metabolizing machines. In plain terms, carbamazepine is a heavyweight CYP enzyme inducer that can shave off a big chunk of many co‑prescribed medicines.
Why carbamazepine matters as a CYP inducer
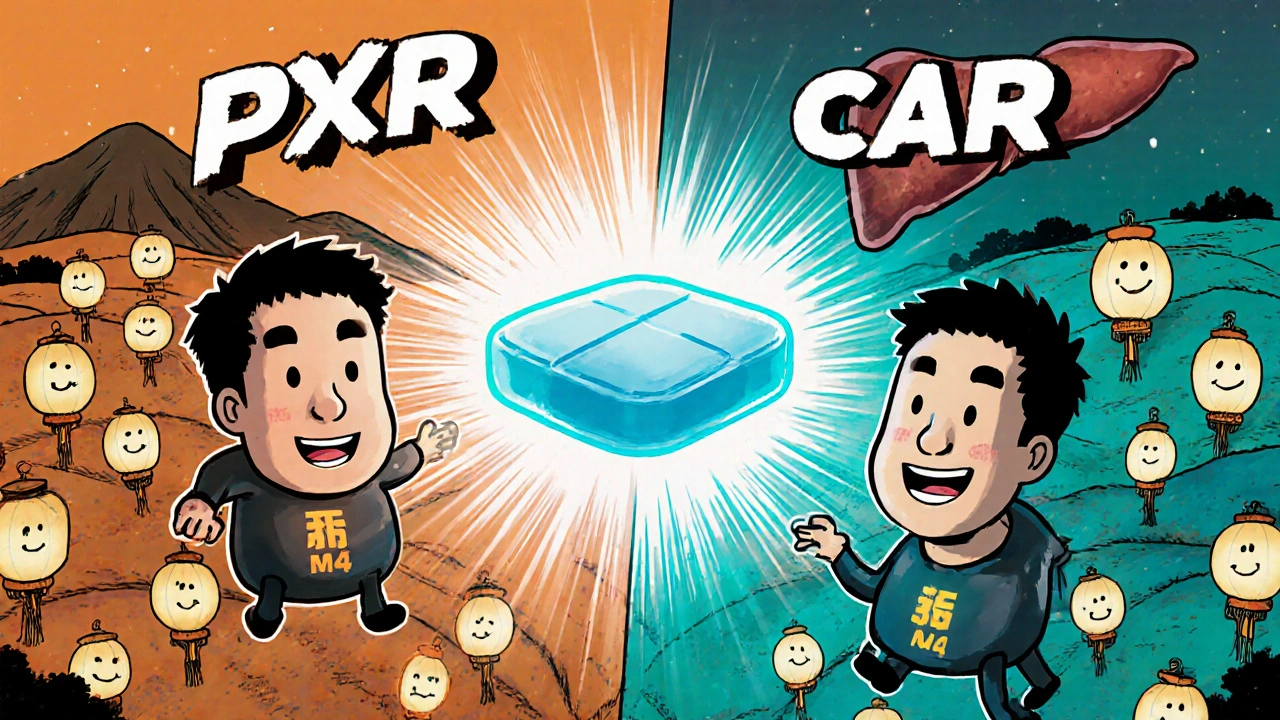
Carbamazepine activates two nuclear receptors - the Pregnane X receptor (PXR) and the Constitutive androstane receptor (CAR). Once switched on, these receptors boost the liver’s production of several cytochrome P450 enzymes, most notably CYP3A4 and CYP2B6. Together they handle roughly half of all prescription drugs.
Studies from Fuhr et al. (2021) report EC50 values for CYP3A4 induction ranging from 4.3 to 108 µM, with an average around 20 µM. That means once carbamazepine hits therapeutic levels, the enzyme spike is significant and sustained.
Auto‑induction: carbamazepine’s own sneaky trick
Unlike many drugs, carbamazepine speeds up its own clearance. Within three to four weeks of daily dosing, blood levels can drop 30‑50 % because the body has cranked up the very enzymes that break it down. In practice, a patient starting at 200 mg twice daily often needs a bump to 800‑1,200 mg per day after a month to stay in the therapeutic window of 4‑12 µg/mL.
The International League Against Epilepsy (2019) recommends baseline therapeutic drug monitoring, then checks at two and four weeks to catch this dip before seizures break out again.
How carbamazepine reshapes other drugs’ exposure
Because CYP3A4 is the workhorse behind many meds, carbamazepine can slash their effectiveness. Here are a few real‑world examples:
- Statins: In a carbamazepine‑simvastatin study, simvastatin’s AUC fell to 26 % of normal - a 74 % reduction that can undermine cholesterol control.
- Oral contraceptives: Ethinyl estradiol exposure drops 50‑70 %, raising the risk of unintended pregnancy.
- Warfarin: INR can fall dramatically, often requiring a 50‑100 % dose increase to keep anticoagulation in range.
- Benzodiazepines such as alprazolam: When carbamazepine is stopped, the reduced enzyme activity can leave patients with excess sedation unless the dose is tapered.
Clinicians frequently see patients needing dose adjustments for these and over 30 % of interactions involve anticoagulants, antidepressants, or immunosuppressants (Perucca et al., 2017).
Head‑to‑head: carbamazepine vs other inducers
| Inducer | Primary CYP enzymes induced | Typical reduction in a sensitive CYP3A4 substrate (AUC %) | Time to maximal induction | Notable side‑effects |
|---|---|---|---|---|
| Carbamazepine | CYP3A4, CYP2B6 | 60‑80 % ↓ | ≈14 days | Auto‑induction, rash, Stevens‑Johnson risk |
| Rifampicin | CYP3A4, CYP2C9, CYP2C19 | 70‑90 % ↓ | 5‑7 days | Hepatotoxicity, orange‑colored fluids |
| Phenytoin | CYP3A4, CYP2C9 | 55‑65 % ↓ | ≈10 days | Gingival hyperplasia, hirsutism |
Carbamazepine’s slower onset gives clinicians a bit more wiggle room to monitor levels, but the auto‑induction curve adds a moving target that newer agents lack.
Practical steps for safe prescribing
- Start with a low dose (e.g., 200 mg BID) and titrate up over 2‑3 weeks while checking plasma levels.
- Before adding a new drug, review its primary metabolic pathway. If it relies on CYP3A4, CYP2B6, CYP2C9, or CYP2C19, anticipate a 30‑80 % drop in exposure.
- Consider pre‑emptive dose reductions for high‑risk drugs (e.g., lower warfarin dose by 25‑50 % and re‑check INR within 3‑5 days).
- Use therapeutic drug monitoring for the victim drug whenever possible - many labs offer rapid assays for statins, oral contraceptives metabolites, and certain antipsychotics.
- If carbamazepine must be stopped, taper the victim drug’s dose down by 25‑50 % over 2‑4 weeks to avoid toxicity.
- Document the interaction in the patient’s medication list and flag it for future prescribers.
These steps cut down surprise breakthrough seizures and adverse drug events, which are the two biggest pitfalls reported on professional forums like r/neurology and r/pharmacy.
Emerging tools and future directions
The Open Systems Pharmacology platform now hosts a publicly available PBPK model for carbamazepine DDIs. While the model still shows a 30 % prediction error in a quarter of cases, it’s a valuable starting point for complex regimens.
Two promising developments aim to sidestep the induction problem altogether:
- Extended‑release carbamazepine‑ASP (FDA‑approved 2023) smooths plasma peaks, reducing the magnitude of CYP induction by about a third.
- Eslicarbazepine, a carbamazepine analog, shows an 80 % lower CYP3A4 induction potential in Phase III trials, making it a potential substitute for patients on multiple CYP‑metabolized drugs.
Meanwhile, a NIH‑backed trial (NCT05678901) is testing pharmacogenetic‑guided dosing based on PXR and CAR polymorphisms. Early data suggest that patients with high‑activity receptor variants may need a 20‑30 % lower carbamazepine dose to stay within therapeutic range.
Bottom line for clinicians
Carbamazepine’s dual role as a perpetrator and victim in drug‑drug interactions makes it one of the most challenging agents to manage. By understanding its induction timeline, identifying high‑risk co‑medications, and applying proactive monitoring, prescribers can keep seizures under control without jeopardizing the efficacy of other therapies.
How long does it take for carbamazepine to reach full enzyme‑inducing effect?
Full induction usually appears after about 14 days of consistent dosing, as measured by urinary 6β‑hydroxycortisol ratios and plasma 4β‑hydroxycholesterol levels.
Can I use carbamazepine with oral contraceptives safely?
Not without extra protection. Carbamazepine can cut estrogen exposure by half, so a backup barrier method or a higher‑dose contraceptive is recommended.
What monitoring is needed when starting carbamazepine?
Check plasma carbamazepine levels at baseline, then at 2 weeks and 4 weeks. Also monitor INR if the patient is on warfarin and lipid panels if on statins.
Is extended‑release carbamazepine a better choice for patients on many medications?
The extended‑release formulation flattens peak concentrations, which reduces but does not eliminate induction. It’s a reasonable option when drug‑interaction risk is moderate.
How should I adjust other drugs when stopping carbamazepine?
Decrease the dose of CYP3A4 or CYP2B6 substrates by about 25‑50 % over 2‑4 weeks and reassess clinical response or drug levels.
When we talk about carbamazepine it feels like we’re peering into a tiny universe where enzymes are the hidden gears of our bodies.
Each dose nudges the pregnane X receptor and the constitutive androstane receptor, like tiny switches that flicker on a dimmer.
The result is a cascade of CYP3A4 and CYP2B6 production that can dramatically rewrite the story of any co‑prescribed medication.
Imagine a painter who suddenly decides to use a brighter palette; the same canvas, but the colors are blander to the eye.
Clinicians often confront this reality when a patient’s statin levels drop to a whisper after a month on carbamazepine.
The paradox is that the drug we rely on to calm seizures also robs other drugs of their potency.
What makes carbamazepine even more fascinating is its own auto‑induction, a self‑defeating loop that erodes its own plasma concentration.
Within three weeks the body can accelerate its clearance by up to fifty percent, demanding a dose hike that feels like chasing a moving target.
Therapeutic drug monitoring becomes not just a suggestion but a compass in this shifting landscape.
If we fail to check levels at two and four weeks, we risk the patient slipping back into seizures, a scenario no one wants.
The interaction with oral contraceptives is another cautionary tale-half the estrogen exposure can mean an unplanned pregnancy.
Warfarin patients may find their INR plummeting, forcing a sudden dose increase that can feel like walking a tightrope.
In the grand scheme, carbamazepine teaches us humility; it reminds us that pharma is a conversation, not a command.
Future formulations like extended‑release carbamazepine‑ASP or eslicarbazepine promise a softer touch on the enzyme system.
Until those become mainstream, the best we can do is to anticipate, monitor, and adjust with vigilant care.
So, in the end, carbamazepine’s dual identity as both perpetrator and victim is a reminder that medicine is always a dance between chemistry and humanity.