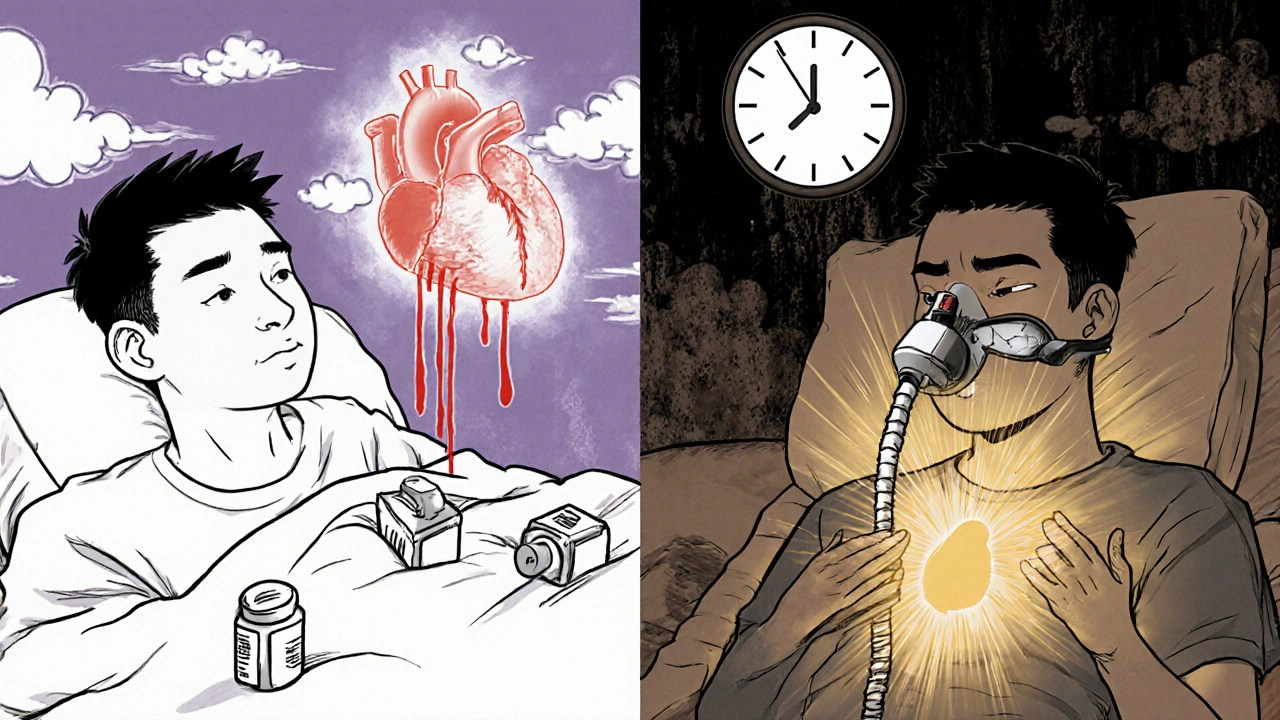
When you stop breathing in your sleep - even for just 10 seconds - your body panics. Your heart pounds. Your blood pressure spikes. And over time, this nightly stress can silently damage your heart, arteries, and brain. Sleep apnea isn’t just loud snoring or tired days. It’s a hidden driver of high blood pressure, heart attacks, and strokes - especially if you’re under 40.
What Sleep Apnea Really Does to Your Body
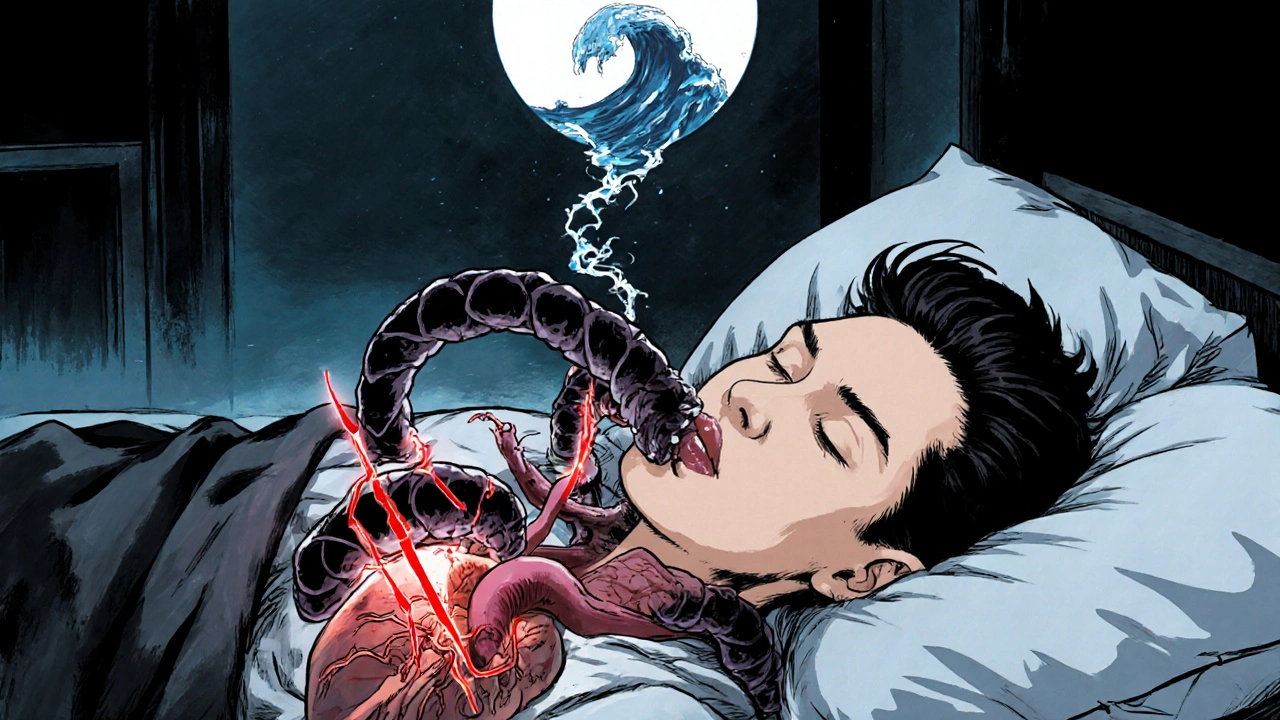
Obstructive sleep apnea (OSA) happens when your throat muscles relax too much during sleep, blocking your airway. These blockages can happen 15, 30, even 100 times an hour. Each time, your oxygen drops. Your brain wakes you up - just enough to breathe, but not enough for real rest. This cycle repeats all night. And every time it happens, your body floods with stress hormones like adrenaline.
Studies show people with moderate to severe OSA have 2 to 4 times higher levels of these stress chemicals during sleep than people who breathe normally. That constant surge is what turns a sleep problem into a heart problem.
High Blood Pressure: The Most Common Link
Up to 80% of people with hard-to-treat high blood pressure - the kind that won’t drop even after taking three different medications - also have sleep apnea. That’s not a coincidence. The repeated drops in oxygen trigger your nervous system to keep your blood pressure high, even when you’re resting.
Normally, your blood pressure drops 10-20% at night. This is called “dipping,” and it’s how your heart gets a break. But in 70-80% of people with OSA, this doesn’t happen. Their blood pressure stays high all night - a pattern called non-dipping. This is one of the strongest predictors of future heart attacks and strokes.
Research from the Wisconsin Sleep Cohort found that people with untreated OSA are 2 to 3 times more likely to develop high blood pressure within just 4-5 years. And it’s not just older adults. Adults aged 20-40 with sleep apnea have a 45% higher risk of hypertension than their peers without it. For younger people, sleep apnea doesn’t just add risk - it accelerates it.
Heart Disease, Heart Attacks, and the Midnight Danger
People with moderate to severe OSA have a 30% higher risk of coronary artery disease and a 60% higher risk of fatal heart events. Why? The same stress hormones that raise blood pressure also cause inflammation, damage blood vessel linings, and make blood more likely to clot.
One startling finding: 26.5% of heart attacks in people with sleep apnea happen between midnight and 6 a.m. - compared to just 16.5% in those without it. That’s because your body is under maximum stress during those apnea episodes. Your heart is working harder, your blood pressure is elevated, and your arteries are under strain.
OSA also makes existing heart disease worse. If you’ve had a heart attack, untreated sleep apnea doubles your chance of having another one. And if you’re on medications like beta-blockers or statins, sleep apnea can make them less effective.
Stroke Risk Skyrockets
People with sleep apnea are 2.5 times more likely to have a first stroke - and 3.2 times more likely to have a second one. The worse the oxygen drops during sleep (especially if levels fall below 90% for more than 12% of the night), the higher the risk of dying from that stroke.
Why? Repeated hypoxia (low oxygen) damages the brain’s blood vessels and triggers clots. It also worsens atrial fibrillation - a dangerous irregular heartbeat that’s a major cause of stroke. In fact, nearly half of people with intermittent atrial fibrillation have undiagnosed sleep apnea. Treating the sleep apnea can reduce the chance of AFib coming back after treatment by up to 50%.
Heart Failure: A Dangerous Loop
Between 40% and 60% of people with heart failure also have sleep apnea. And it’s not just a side effect - it makes heart failure worse. OSA increases the risk of developing heart failure by 140%.
Here’s the vicious cycle: weak heart → fluid builds up in the lungs → airway gets blocked → apnea happens → oxygen drops → heart works harder → heart gets weaker. It’s a downward spiral. People with heart failure and untreated OSA have higher hospitalization rates, worse symptoms, and shorter life expectancy.
Why CPAP Doesn’t Always Fix Everything
Continuous Positive Airway Pressure (CPAP) machines are the gold standard treatment. They keep your airway open with gentle air pressure. But here’s the catch: only 46% of people use CPAP enough to get real benefits - meaning at least 4 hours a night, 70% of nights.
CPAP can reduce blood pressure, but only by 2-3 mmHg on average. That’s not enough to make a big difference for someone with severe hypertension. However, it does cut stroke recurrence by 37% and improves heart failure outcomes - especially for central sleep apnea.
The real problem? Many people don’t feel better right away. They think CPAP isn’t working. But the benefits are long-term. It’s not about feeling more rested tomorrow - it’s about avoiding a heart attack five years from now.
Who Should Be Screened - And How
The American Heart Association says: if you have high blood pressure, atrial fibrillation, heart failure, stroke, or coronary disease - get tested for sleep apnea. Especially if your treatment isn’t working.
Doctors can use a simple tool called the STOP-Bang questionnaire. It asks about snoring, tiredness, observed breathing pauses, high blood pressure, BMI, age, neck size, and gender. It catches 84% of moderate to severe cases. No sleep lab needed.
Home sleep tests are also reliable for moderate to severe OSA - they’re 85-90% accurate. But they often miss mild cases. If you’re young, overweight, and have high blood pressure, even a mild case can be dangerous.
The Hidden Crisis in Younger Adults
Most people think sleep apnea is an older adult problem. It’s not. The UT Southwestern study found that adults under 40 with sleep apnea symptoms had much higher rates of hypertension, diabetes, and metabolic syndrome than older adults with the same condition.
For younger people, sleep apnea doesn’t just add risk - it fast-tracks it. A 35-year-old with untreated OSA might develop heart disease normally seen in someone 60. That’s why screening should start earlier - especially if you’re overweight, snore loudly, or wake up gasping.
What You Can Do Now
If you snore, feel exhausted during the day, or have high blood pressure that won’t go down - don’t wait. Talk to your doctor. Ask for a sleep apnea screening. Even if you think it’s "just snoring," it might be your heart’s warning sign.
Weight loss helps - even 10% can cut apnea episodes in half. Sleeping on your side, avoiding alcohol before bed, and quitting smoking also reduce severity. But if you have moderate to severe OSA, CPAP is still the most proven way to protect your heart.
And if you’re already on heart medication - know this: untreated sleep apnea can make those drugs less effective. Treating your sleep could be the missing piece in your heart health plan.
Can sleep apnea cause high blood pressure even if I’m not overweight?
Yes. While obesity is the biggest risk factor - accounting for 70% of cases - sleep apnea can happen in thin people too. Structural issues like a narrow airway, large tonsils, or jaw position can block breathing. Anyone who snores loudly, wakes up gasping, or has unexplained high blood pressure should be screened, regardless of weight.
If I use CPAP, will my blood pressure go back to normal?
Not always. CPAP typically lowers blood pressure by just 2-3 mmHg on average. That’s not enough to eliminate hypertension, especially in severe cases. But it reduces nighttime spikes, improves heart rhythm, and cuts stroke risk by 37%. The goal isn’t just lowering numbers - it’s protecting your heart and brain from the damage caused by repeated oxygen drops.
Is sleep apnea linked to heart failure?
Yes - and it’s a two-way street. About half of people with heart failure also have sleep apnea. OSA increases the risk of developing heart failure by 140%. At the same time, heart failure can cause fluid buildup that blocks the airway, making apnea worse. Treating OSA improves heart function, reduces hospital visits, and helps patients live longer.
Can sleep apnea cause a stroke?
Absolutely. People with untreated sleep apnea are 2.5 times more likely to have a first stroke and 3.2 times more likely to have a second one. The repeated drops in oxygen cause inflammation, blood vessel damage, and clotting. The risk is highest when oxygen levels fall below 90% for more than 12% of the night. Screening and treating sleep apnea can cut stroke risk significantly.
Should I get tested for sleep apnea if I have atrial fibrillation?
Yes - and quickly. Nearly half of people with paroxysmal atrial fibrillation have undiagnosed sleep apnea. If you have AFib and don’t treat your sleep apnea, your chances of the irregular heartbeat returning after treatment - like ablation - are 30% higher. Treating OSA improves AFib outcomes and reduces the need for repeat procedures.
Final Thought: Your Heart Doesn’t Sleep - But Your Airway Might
Sleep apnea is not a lifestyle issue. It’s a cardiovascular emergency in slow motion. Every time you stop breathing at night, your heart is fighting for survival. The damage builds silently - until it doesn’t.
If you’re tired, snoring, or have high blood pressure that won’t budge - don’t ignore it. Get tested. Your heart is counting on it.
I never thought snoring could be this dangerous. My dad had it for years and just shrugged it off. Now I’m pushing him to get tested. His BP’s been through the roof since last year.