Anticholinergic Burden Calculator
Medication Entry
Your Medications
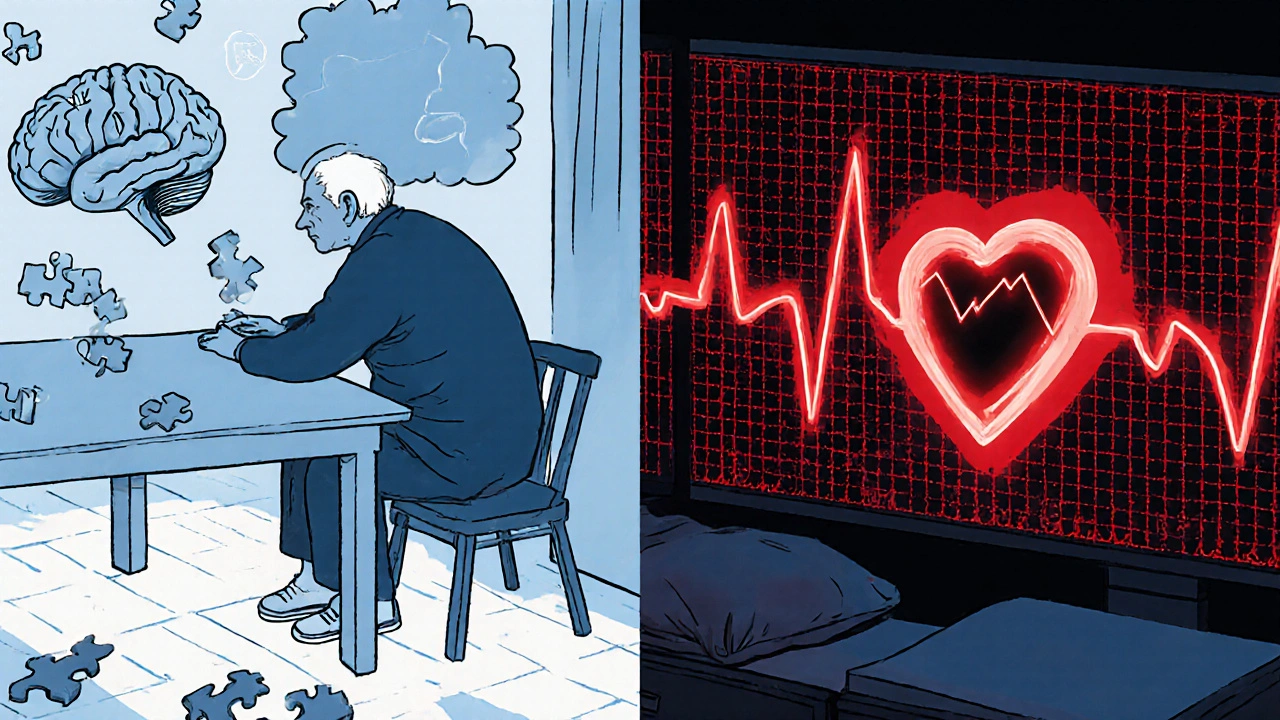
When we talk about tricyclic antidepressants are a class of older antidepressants that inhibit serotonin and norepinephrine reuptake while also blocking muscarinic acetylcholine receptors. They remain useful for treatment‑resistant depression and certain pain syndromes, but their strong anticholinergic activity creates a hidden danger-especially for middle‑aged and older adults.
Understanding the anticholinergic burdenthe cumulative effect of drugs that block acetylcholine receptors is the first step toward protecting cognition and the heart. The burden is quantified with tools such as the Anticholinergic Cognitive Burden (ACB) Scale, which assigns scores of 1‑3 based on how strongly a medication blocks muscarinic receptors.
How Anticholinergic Burden Is Measured
- Three validated scales dominate clinical practice: the ACB Scale, the ACB Calculator, and Medichec.
- Each medication receives a score of 1 (possible activity), 2 (moderate activity), or 3 (definite high activity).
- A total ACB score of 3 or higher flags a patient as being at significantly increased risk for adverse cognitive and cardiac outcomes.
For example, amitriptyline and nortriptyline-two of the most commonly prescribed tricyclic antidepressants-consistently earn an ACB score of 3 across all three tools, placing them in the highest risk tier.
Cognitive Risks: What the Numbers Mean
Research highlighted in the NICE guideline NG97 (2022) links ACB ≥ 3 with a 54 % higher chance of developing dementia over a seven‑year span. A landmark JAMA Internal Medicine cohort of 3,434 adults over 65 showed that the presence of a single high‑scoring drug (ACB=3) was enough to drive that risk.
Why does this happen? Blocking acetylcholine interferes with the neurotransmitter system that supports memory and attention. Over time, patients experience:
- Reduced short‑term memory and slower information processing.
- Fluctuating attention that can be mistaken for early‑stage Alzheimer’s disease.
- Difficulty with executive tasks, often leading clinicians to misdiagnose dementia.
Real‑world testimony mirrors the data. On the AARP forums, 68 % of respondents over 65 reported two or more anticholinergic side‑effects, and one third said memory problems were severe enough to consider stopping their medication.
Cardiac Risks: The QT and QRS Connection
Beyond the brain, QT prolongationan elongation of the heart’s electrical repolarization phase that can trigger dangerous arrhythmias is a well‑documented hazard of TCAs. Amitriptyline, at therapeutic doses, can lengthen the QRS complex by 10‑25 % and the QT interval by up to 2.8 times compared with sertraline, a typical SSRI.
The mechanism mirrors class 1A antiarrhythmics: sodium channel blockade reduces contractility by roughly 15‑20 % while increasing myocardial irritability. In overdose situations, QRS widening can exceed 50 %, a sign of life‑threatening toxicity.
Clinicians report palpitations, dizziness, and emergency‑room visits for arrhythmias in up to 32 % of older patients taking TCAs, according to a 2022 Mended Hearts support‑group survey.
Side‑by‑Side Comparison: TCAs vs. Modern Antidepressants
| Drug Class | Typical ACB Score | QT Prolongation Risk | Common Clinical Use |
|---|---|---|---|
| Amitriptyline (TCA) | 3 | High (≈2.8× SSRI) | Severe depression, neuropathic pain |
| Nortriptyline (TCA) | 3 | High (slightly lower than amitriptyline) | Depression, chronic pain |
| SSRIs (e.g., sertraline) | 0‑1 | Low | First‑line depression |
| SNRIs (e.g., duloxetine) | 0‑1 | Low | Depression & pain |
The table makes it clear why most clinicians now reserve TCAs for cases where SSRIs or SNRIs have failed. The anticholinergic and cardiac profiles of modern agents are far gentler, translating into lower rates of dementia and arrhythmia.
Practical Steps to Assess and Reduce Burden
For any patient over 50, a systematic medication review should become routine. Follow this checklist:
- Run an ACB calculation using an online calculator or integrated EHR tool.
- Identify all prescription and over‑the‑counter drugs with anticholinergic activity (e.g., diphenhydramine, chlorphenamine).
- If total ACB ≥ 3, prioritize tapering or switching high‑scoring agents.
- Choose alternatives with ACB ≤ 1-such as duloxetinean SNRI with minimal anticholinergic effect for depression and pain.
- Implement a tapering schedule: reduce the TCA dose by 10‑25 % every 1‑2 weeks over 4‑8 weeks to avoid withdrawal.
- Re‑assess cognition after 3 months using the Mini‑Mental State Examinationa quick screen for global cognitive function (MMSE).
- Monitor ECG at baseline and after any dose change to catch QT or QRS prolongation early.
Structured deprescribing programs in the UK have cut anticholinergic burden in 78 % of eligible patients, with 63 % showing measurable cognitive improvement within six months.

When Is a TCA Still the Right Choice?
Guidelines don’t ban TCAs outright. They remain valuable for:
- Severe, treatment‑resistant depression where other agents have failed.
- Neuropathic pain conditions that respond poorly to SSRIs/SNRIs.
- Patients without cardiac disease and who are under regular ECG surveillance.
Even in these scenarios, the decision should involve a shared‑decision‑making discussion, weighing the high anticholinergic score against the therapeutic need.
Future Directions: Reducing the Burden with Technology
AI‑driven medication review tools are already being piloted in UK trusts. They automatically calculate ACB scores as clinicians prescribe, flagging high‑risk combinations in real time. As these systems mature, we can expect:
- Fewer inadvertent high‑burden prescriptions.
- Earlier detection of cognitive decline linked to medication.
- Integration with cardiac monitoring platforms to alert for QT changes.
Regulatory bodies like the Beers Criteria have already upgraded their warnings on TCAs, urging avoidance in adults over 65 unless benefits clearly outweigh risks. The market forecast predicts TCA use for depression to drop below 3 % in the United States by 2028.
Key Takeaways
- anticholinergic burden from TCAs is a major, measurable risk factor for dementia and heart rhythm problems.
- An ACB score of 3 (the level TCAs consistently hit) triples the odds of cognitive decline.
- Cardiac monitoring is essential; amitriptyline can markedly prolong QT and QRS intervals.
- When possible, switch to low‑burden agents like SSRIs or SNRIs and apply a structured taper.
- Emerging AI tools promise to make burden assessment a routine part of prescribing.
What is an ACB score and how is it calculated?
The Anticholinergic Cognitive Burden (ACB) score rates each medication from 1 (possible anticholinergic activity) to 3 (definite high activity). Clinicians sum the scores of all drugs a patient takes; a total of 3 or more signals a high risk for cognitive and cardiac adverse effects.
Why do tricyclic antidepressants have such high anticholinergic scores?
TCAs block muscarinic acetylcholine receptors as part of their pharmacologic profile. This antimuscarinic action is strong enough to earn a rating of 3 on the ACB Scale, the highest possible score.
How does anticholinergic burden affect the heart?
High‑burden drugs can prolong the QT interval and widen the QRS complex, increasing the chance of ventricular arrhythmias. Amitriptyline, for example, raises QT prolongation risk by about 2.8 times compared with sertraline.
When is it safe to keep a patient on a TCA?
A TCA may be justified for treatment‑resistant depression or neuropathic pain in patients without existing cardiac disease, who can undergo regular ECG monitoring, and when alternative agents have failed.
What steps should I take to deprescribe a TCA?
Start with an ACB calculation, identify lower‑burden alternatives, then taper the TCA by 10‑25 % every 1‑2 weeks over 4‑8 weeks. Re‑evaluate cognition with the MMSE and monitor ECG after each dose reduction.
Listen up, the anticholinergic load of TCAs is a textbook case of pharmacology gone rogue. Those drugs slam the muscarinic receptors like a wrecking ball, and the fallout hits both brain and heart. A total ACB score of three isn’t just a number – it’s a red flag that should scream for a faster alternative. Forget the nostalgic hype; modern SSRIs and SNRIs keep the cognitive train on the right tracks. If you’re still prescribing amitriptyline without a strict ECG watch, you’re practically courting disaster.