Liver Function Dose Adjuster
Adjust Medication Doses for Liver Disease
Based on clinical guidelines for liver impairment. Select your drug and liver function to see recommended dose adjustments.
When your liver isn’t working right, even a normal dose of a common medication can become dangerous. This isn’t theory-it’s daily reality for millions. In the U.S. alone, over 22 million people live with chronic liver disease, and for many, the medications they take to manage other conditions are quietly building up in their system. Why? Because the liver can’t clear them the way it used to.
How the Liver Normally Processes Drugs
Your liver is the body’s main drug-processing plant. It doesn’t just break down toxins-it handles most prescription meds. Two main systems do the work: enzymes (especially the CYP450 family) and transport proteins. These tag drugs for elimination, either by turning them into inactive forms or shuttling them into bile for excretion. For drugs like warfarin, diazepam, or morphine, the liver is the only exit route.
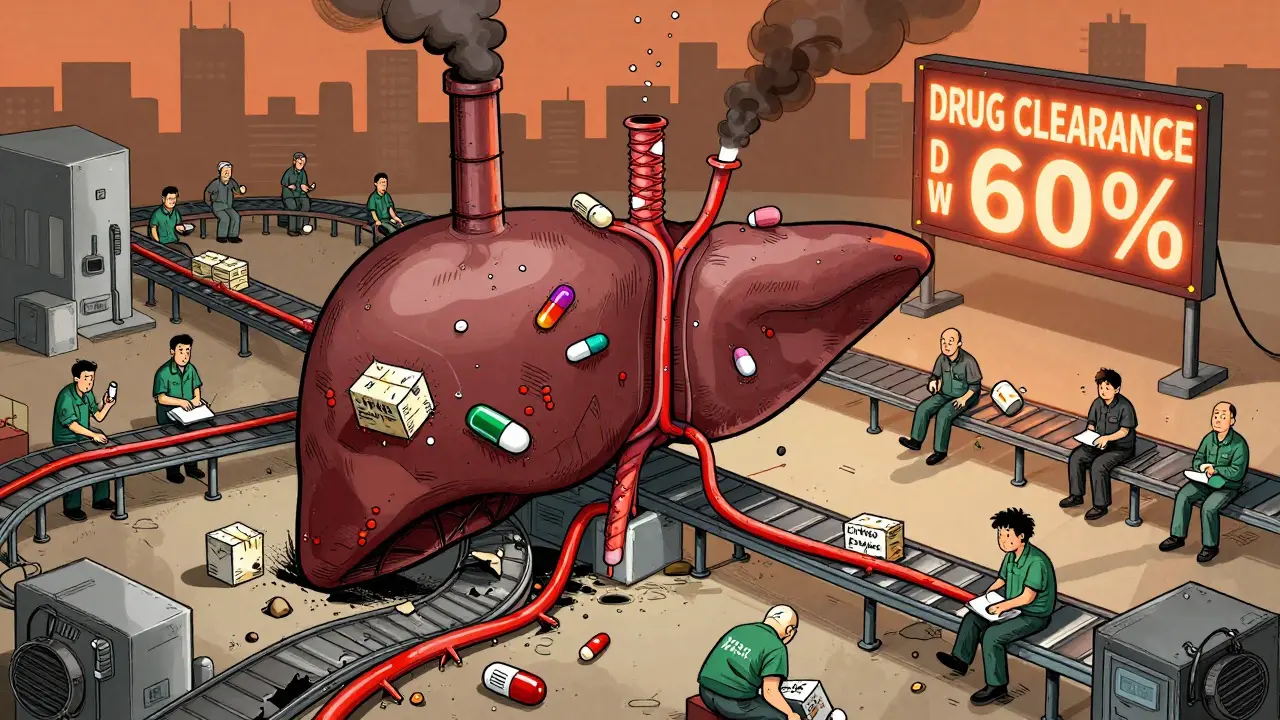
Not all drugs are processed the same way. Some, like fentanyl, are high-extraction drugs-meaning their clearance depends mostly on how much blood flows through the liver. Others, like lorazepam or methadone, are low-extraction drugs, where the liver’s metabolic capacity matters more than blood flow. About 70% of commonly prescribed drugs fall into this second group. That’s critical: if your liver’s enzymes are damaged, these drugs stick around longer, and their effects pile up.
What Happens When the Liver Fails
In cirrhosis or advanced liver disease, multiple systems break down at once. Blood flow through the liver drops by 30-50%. Liver cells shrink and die. Scarring creates shunts-bypass roads that let blood skip the liver entirely. Up to 40% of blood can flow around the liver instead of through it. That means oral drugs get absorbed directly into the bloodstream without being broken down first. The result? Higher drug levels than expected.
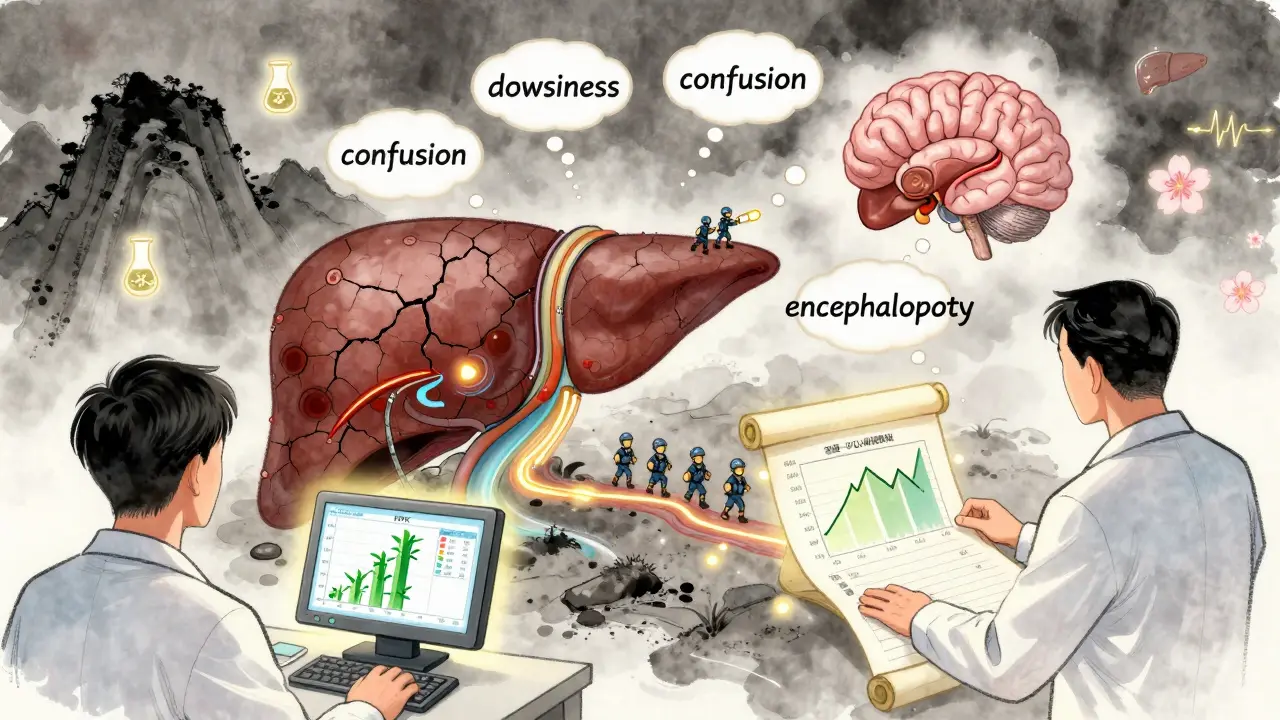
Enzymes like CYP3A4 and CYP2E1 drop in activity by 30-60%. Transporters like OATP1B1, which pull drugs into liver cells, fall by 50-70%. Even bile flow slows. All of this adds up to one thing: drugs aren’t cleared. Their half-lives stretch. A drug that normally lasts 6 hours might now last 12 or 18. And since many of these drugs act on the brain-opioids, benzodiazepines, sedatives-the consequences are severe.
Real-World Risks: When Normal Doses Become Dangerous
Patients with liver disease don’t just metabolize drugs slower-they’re more sensitive to their effects. Studies show cerebral sensitivity to opioids and sedatives increases by 30-50%. A standard dose of morphine that’s safe for a healthy person can trigger drowsiness, confusion, or full-blown hepatic encephalopathy in someone with cirrhosis. That’s not rare. It’s predictable.
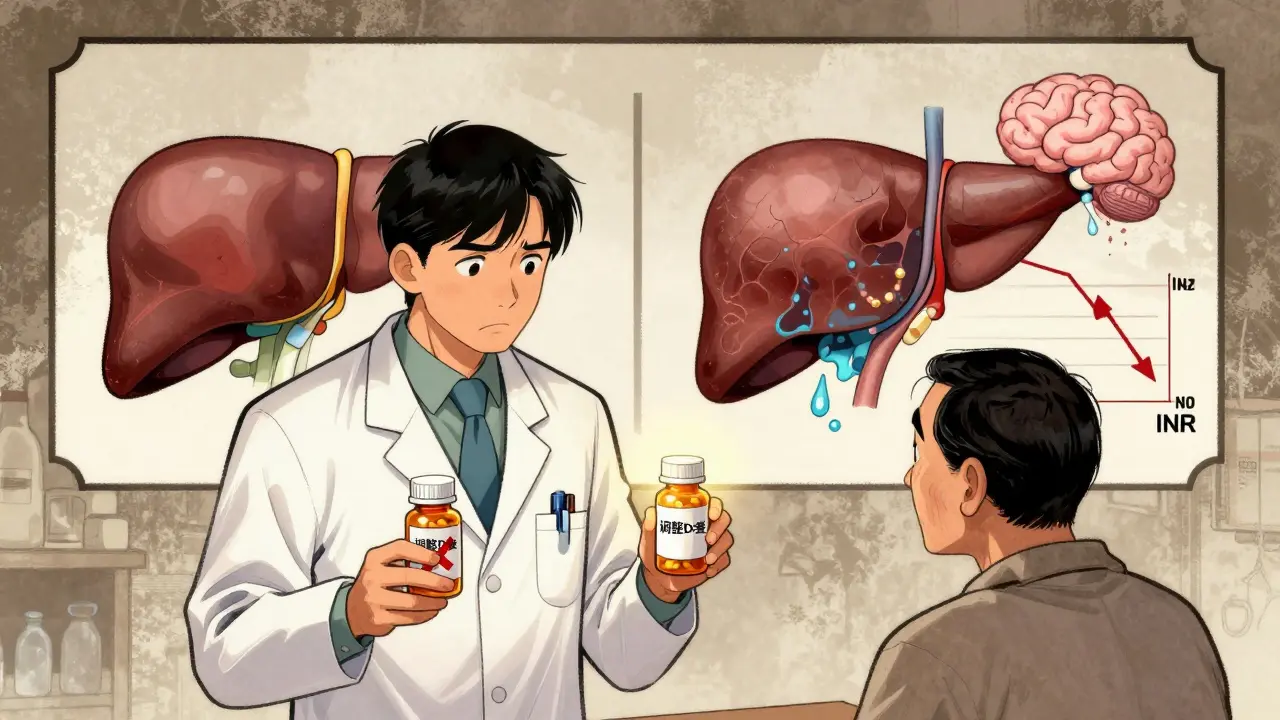
Warfarin, a blood thinner, is another classic case. In cirrhosis, its clearance drops by 30-50%. If you keep giving the same dose, the INR skyrockets. Bleeding risk jumps. The fix? Reduce the dose by 25-40%. But many clinicians still use standard dosing-because they don’t know the numbers, or because they assume liver disease always means higher risk, which isn’t always true.
And then there’s the myth that all drugs are riskier in liver disease. Data from the Merck Manual shows adverse drug reactions aren’t significantly more common in advanced liver disease (odds ratio 1.15). But here’s the catch: patients tolerate those reactions far worse. Their bodies have no reserve. A mild side effect in a healthy person can be life-threatening in someone with cirrhosis.
Which Drugs Are Safe? Which Aren’t?
Not every drug needs a dose change. The FDA says if a drug is cleared almost entirely by the kidneys-with no liver involvement-you’re probably fine. Sugammadex, for example, is 96% excreted in urine. Even in liver transplant patients, no dose reduction is needed. But recovery from muscle paralysis takes 40% longer, so monitoring matters.
For drugs that are metabolized by the liver, the rule is simple: if it’s cleared by the liver and has a narrow therapeutic window, assume it’s dangerous unless proven otherwise. Benzodiazepines are a perfect example. Diazepam has active metabolites that hang around for days. In cirrhosis, reduce the dose by 50-70%. Lorazepam? No active metabolites. Just cut the dose by 25-40%. The difference is huge.
Antibiotics like ceftriaxone are another trap. Standard doses in cirrhotic patients can cause peak concentrations 40-60% higher than normal. That’s why 68% of hepatologists report frequent dosing errors with antibiotics in these patients.
How Doctors Measure Liver Function-And Why It’s Not Enough
Many doctors still rely on a single lab value: ALT, AST, or bilirubin. That’s not enough. The liver is too complex. A patient might have normal enzymes but severe scarring. Or high bilirubin from Gilbert’s syndrome-not liver failure.
The gold standard is the Child-Pugh score. It combines five factors: bilirubin, albumin, INR, ascites, and encephalopathy. Class A (mild), B (moderate), C (severe). For Child-Pugh B, most hepatically cleared drugs need a 25-50% dose reduction. For Class C? 50-75%.
Another tool gaining ground is the MELD score (Model for End-Stage Liver Disease). For every 5-point increase above 10, drug clearance drops by about 15%. That’s useful for predicting how a drug will behave-even if you don’t know the exact enzyme involved.
But here’s the kicker: drug levels don’t always match liver test results. Two people with identical bilirubin levels might clear a drug completely differently. That’s why therapeutic drug monitoring (TDM) is essential for drugs like warfarin, phenytoin, or tacrolimus. You can’t guess. You have to measure.
New Tools Are Changing the Game
For years, dosing in liver disease was guesswork. Now, it’s becoming science. Physiologically based pharmacokinetic (PBPK) modeling uses computer simulations to predict how a drug behaves in a diseased liver. It factors in blood flow, enzyme levels, shunting, and cell loss. Studies show these models predict drug exposure with 85-90% accuracy.
The FDA is catching up. In 2024, they released draft guidance pushing for PBPK modeling in new drug applications. Within five years, 70% of new drug labels will likely include model-based dosing for liver impairment, says Dr. Aleksandra Galetin of the University of Manchester.
Even early-stage fatty liver-MASLD-is now known to reduce CYP3A4 activity by 15-25%. That’s not just for cirrhosis anymore. If you have metabolic syndrome, your liver might already be slowing down your meds.
What You Can Do
If you or someone you care for has liver disease:
- Ask your doctor: “Is this drug cleared by the liver?”
- Ask: “What’s the right dose for my liver function?”
- Ask for a Child-Pugh or MELD score if it hasn’t been done.
- Never assume a dose is safe just because it’s “standard.”
- For narrow-therapeutic-index drugs, ask about therapeutic drug monitoring.
Pharmacists are now playing a bigger role too. Between 2020 and 2023, pharmacist-led dose adjustment services for liver patients increased by 40%. They’re the ones checking for hidden interactions and outdated dosing.
The bottom line: liver disease doesn’t just affect the liver. It affects every pill you take. Ignoring it isn’t negligence-it’s dangerous. But with the right tools and awareness, we can avoid harm. It’s not about avoiding meds. It’s about getting the right dose.
Can I still take painkillers if I have liver disease?
Yes-but not all of them. Acetaminophen (Tylenol) is usually safe at low doses (under 2,000 mg/day) in mild liver disease, but avoid it entirely in severe cirrhosis. NSAIDs like ibuprofen can worsen kidney function and fluid retention, so they’re risky too. Opioids like morphine or oxycodone are dangerous without dose reduction because they can trigger encephalopathy. Always check with your doctor or pharmacist before taking any painkiller.
Do I need to stop all my medications if I have cirrhosis?
No. Most people with liver disease still need their medications-but many need lower doses. Stopping meds can be more harmful than adjusting them. For example, stopping blood pressure or diabetes meds can lead to complications worse than the original liver issue. The goal isn’t to stop drugs. It’s to use the right dose for your liver’s current ability to process them.
Why does my doctor say my blood thinner dose changed even though my INR was fine?
Warfarin is cleared by the liver, and in cirrhosis, its clearance drops by 30-50%. Even if your INR was stable, your liver’s ability to break it down has likely worsened. A dose that worked last month might now cause your INR to rise dangerously. Your doctor isn’t just reacting to one number-they’re adjusting for your changing liver function. Regular monitoring is key.
Are herbal supplements safe if I have liver disease?
Many are not. Herbal products like kava, green tea extract, and some weight-loss supplements are linked to liver injury. Even “natural” doesn’t mean safe. The liver is already under stress. Adding unregulated substances increases the risk of further damage. Always tell your doctor about every supplement you take-even if you think it’s harmless.
Can liver disease affect how my body responds to anesthesia?
Yes. Anesthetics and sedatives are often metabolized by the liver. In advanced liver disease, their effects last longer and can be stronger. This increases the risk of prolonged sedation, breathing problems, or confusion after surgery. Anesthesiologists now routinely check liver function before procedures and adjust doses accordingly. Always inform your surgical team about your liver condition.
Drug metabolism in liver disease isn’t a niche topic. It’s a core part of safe prescribing. With rising rates of fatty liver, hepatitis, and cirrhosis, this isn’t going away. The tools are here. The data is clear. What’s missing is awareness-and that’s something you can change.
Yea right, like anyone in the UK actually gives a damn about liver dosing when we’ve got a NHS that can’t even refill a prescription on time.