When your immune system turns on you, it doesn’t just cause discomfort-it can shut down your life. Autoimmune flares aren’t just bad days. They’re sudden, intense waves of symptoms that make walking, thinking, or even getting out of bed feel impossible. For millions of people with conditions like lupus, rheumatoid arthritis, multiple sclerosis, or Crohn’s disease, flares are the silent enemy that shows up without warning. But understanding what triggers them, how to stop them before they start, and what to do the moment they hit can change everything.
What Exactly Is an Autoimmune Flare?
An autoimmune flare is when your immune system, which should protect you from germs, goes rogue and attacks your own tissues. It’s not just a worsening of symptoms-it’s a full-blown immune storm. During a flare, inflammatory markers like CRP and ESR spike. C-reactive protein (CRP) can jump 30-50% above your normal baseline. Erythrocyte sedimentation rate (ESR) might climb from under 20 mm/hr to over 40 mm/hr. Autoantibody levels often double or triple. But numbers don’t tell the whole story.
People describe flares as sudden, overwhelming fatigue-85% of patients report it. Joint pain so severe it makes typing or holding a cup unbearable. Brain fog so thick you forget your own phone number. Skin rashes that burn. Diarrhea that won’t stop. Or numbness that creeps up your legs. These aren’t random. They’re signals your body is under siege.
Flares vary by disease. In lupus, 68% involve joint or muscle pain, 42% affect the kidneys, and 35% show up as rashes. Rheumatoid arthritis flares often start with morning stiffness lasting over 45 minutes-a 92% predictor. MS relapses might mean blurred vision or leg weakness. Crohn’s flares scream with abdominal pain and diarrhea. Ulcerative colitis? Bloody stools and urgency. Each disease has its own fingerprint, but the pattern is the same: immune system out of control.
The 7 Biggest Triggers of Autoimmune Flares
Flares don’t happen for no reason. Research shows seven clear triggers that push the immune system over the edge.
- Stress: Chronic or acute stress throws cortisol off balance. A 2023 study found acute stress increases flare risk by 40-60% within 72 hours. It’s not just "feeling overwhelmed." It’s your nervous system signaling your immune system to go into overdrive.
- Infections: Viruses are major culprits. Epstein-Barr virus reactivation triggers 22% of lupus flares. Even a common cold can spark a flare in 35% of cases. Your body’s fight against the invader accidentally turns into a war on itself.
- Diet: Gluten triggers symptoms in 99% of celiac patients. High-sodium diets raise MS relapse rates by 30%. Sugar and processed foods fuel inflammation. The Autoimmune Protocol (AIP) diet reduced flare frequency by 42% in rheumatoid arthritis patients.
- UV Radiation: Sunlight isn’t just for tanning. It causes 45% of cutaneous lupus flares. UV rays activate immune cells in the skin, triggering rashes, fatigue, and joint pain.
- Seasonal Changes: Spring and fall bring 37% more flares than summer or winter. Temperature shifts, pollen, and humidity all play a role. It’s not coincidence-it’s climate-driven immune disruption.
- Hormonal Shifts: Pregnancy lowers flare risk for some, but postpartum? That’s when 40% of rheumatoid arthritis patients flare. Estrogen and progesterone swings directly affect immune cell behavior.
- Medication Non-Adherence: Skipping doses causes 28% of preventable flares. Even missing one day of methotrexate or hydroxychloroquine can tip the scales.
And don’t overlook gut health. Microbial dysbiosis contributes to 22% of Crohn’s flares. When your gut bacteria are out of balance, your immune system gets confused-and starts attacking.
How to Prevent Flares Before They Start
Prevention isn’t about perfection. It’s about stacking small, consistent habits that reduce your flare risk.
- UV Protection: Use SPF 50+ sunscreen every 2 hours-even on cloudy days. Wear wide-brimmed hats and UV-blocking clothing. A 2022 study showed this cut lupus skin flares by 52% over a year.
- Stress Management: Mindfulness-based stress reduction (MBSR) cut flares by 35% in a 6-month trial. Just 10 minutes a day of breathing exercises or meditation helps. Don’t wait until you’re overwhelmed. Build it into your routine.
- Dietary Changes: Cut gluten if you’re sensitive. Reduce sodium. Avoid processed foods. Add omega-3s from fish or flaxseed. Vitamin D is critical: keeping levels above 40 ng/mL lowered MS relapses by 32%.
- Medication Adherence: Set phone alarms. Use pill organizers. A 2022 study found smartphone reminders boosted compliance by 65% and cut flares by 28%.
- Track Your Triggers: Use an app or journal. Record sleep, food, stress, weather, and symptoms. 68% of people who tracked for 3 months found personal patterns. One woman noticed her flares spiked after eating dairy. Another found sleep deprivation was her trigger. You can’t fix what you don’t track.
- Pre-Flare Kit: Prepare a kit with ice packs, pain meds, electrolyte drinks, and a list of your meds and doctors. People who used this reported 33% faster recovery.
These aren’t "nice-to-haves." They’re survival tools. The goal isn’t to live perfectly-it’s to live predictably.

Early Intervention: The Game-Changer
Waiting until you’re bedridden is a mistake. Early action cuts flare severity in half.
The Lupus Foundation’s "Flare First Response" protocol shows what works: starting corticosteroids within 24 hours of flare onset reduces hospitalizations by 45% and shortens flare duration by over 6 days. But you have to recognize the warning signs.
Most flares have a "pre-flare" phase-usually 2-3 days before full symptoms hit. You might feel unusually tired. Your joints might ache slightly. Your skin tingles. Your brain feels foggy. These aren’t "just tired." They’re your body’s alarm.
Patients trained to recognize these signs were 37% less likely to have severe flares. Telemedicine programs helped too. Patients who could video-call their rheumatologist at first signs had 22% fewer ER visits and saved 18% on costs.
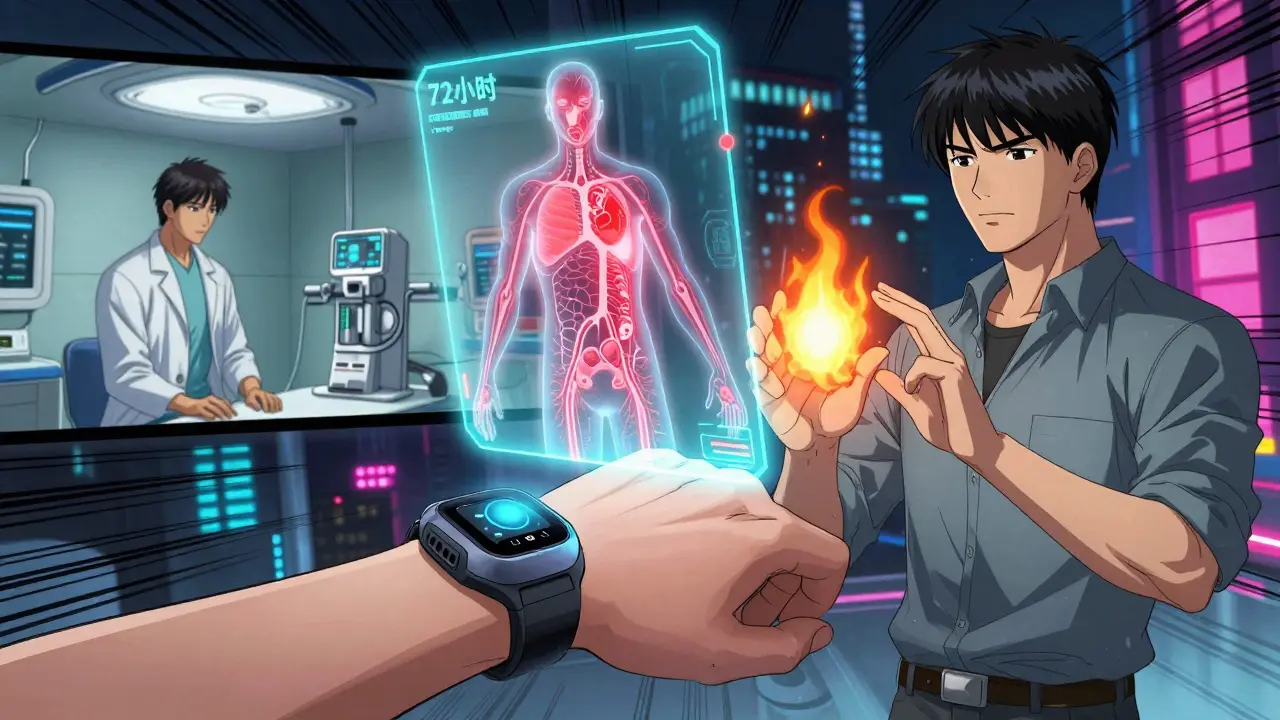
And here’s the future: FlareGuard AI, FDA-approved in 2023, uses wearable sensors to predict flares 72 hours in advance. It tracks heart rate variability, sleep patterns, and activity levels. In trials, it was 76% accurate. The NIH’s new initiative is even more promising-using blood and gene markers to predict lupus flares 14 days ahead with 82% accuracy.
You don’t need to wait for disaster. You can intercept it.
What Experts Are Saying
Dr. William Robinson from Stanford says flares aren’t random-they’re the result of immune networks crossing a threshold. The key? Catch them before they cross it.
The American College of Rheumatology now says patient-reported symptoms matter as much as lab results. One study found 30% of patients with normal CRP and ESR still felt terrible. Your experience counts.
Dr. Victoria Fragiadakis at UCSF is pushing for "serial immune profiling"-regular blood tests to spot immune changes before symptoms appear. Imagine knowing you’re about to flare before you even feel it.
But there’s a warning: overusing steroids. Dr. David Pisetsky points out 65% of patients on frequent steroid bursts develop osteoporosis within 5 years. Steroids are a tool, not a crutch. They’re for emergencies, not daily use.
Real-Life Challenges
Patients say the hardest parts aren’t the pain-they’re the isolation. 78% say flares are unpredictable. 67% feel misunderstood at work. 58% struggle to get timely appointments.
On Reddit’s r/Autoimmune community, 72% of users called brain fog the most disabling symptom. It took 3-5 days for many to realize they were in a flare. That delay costs time, energy, and opportunity.
But there’s hope. Those who tracked triggers, used pre-flare kits, and acted fast had faster recoveries. The best advice from patients? "Track everything. Don’t wait. Speak up. You know your body better than anyone."
What’s Next
The future of flare management is personal. No more one-size-fits-all. We’re moving toward immune phenotyping-mapping your unique immune signature to predict and prevent flares before they happen. Early trials show 50% fewer flares with tailored plans.
Technology is catching up. Wearables, AI, and blood biomarkers will soon give us early warnings. But the most powerful tool remains: awareness. Knowledge. Action.
Autoimmune flares aren’t inevitable. They’re manageable. You don’t need to live in fear of the next one. You need to know your triggers, act early, and protect your body like the only one you’ve got.
Can autoimmune flares be completely prevented?
No, flares can’t be completely prevented-autoimmune diseases are chronic and unpredictable. But their frequency and severity can be dramatically reduced. Studies show consistent stress management, medication adherence, UV protection, and dietary changes can cut flare rates by 30-50%. The goal isn’t zero flares-it’s fewer, milder, and shorter ones.
How do I know if I’m having a flare or just a bad day?
A bad day feels like fatigue or achiness that passes. A flare lasts longer, gets worse, and often includes new symptoms. If you’re unusually tired for more than 2-3 days, have joint swelling you haven’t had before, develop a rash, or experience brain fog that interferes with daily tasks, it’s likely a flare. Track your symptoms over time-you’ll start recognizing your personal pattern.
Is stress really that big of a trigger?
Yes. Stress doesn’t just make you feel tired-it changes your immune system. Cortisol, your stress hormone, can suppress immune regulation and trigger inflammation. Studies show acute stress increases flare risk by 40-60% within 72 hours. Managing stress isn’t optional-it’s medical.
Do I need to follow a strict diet forever?
Not necessarily. The Autoimmune Protocol (AIP) is a temporary elimination diet designed to identify triggers. After 30-90 days, you reintroduce foods one at a time. Many people find they can tolerate small amounts of certain foods again. The goal is personalization, not perfection. If gluten makes you sick, avoid it. If dairy doesn’t affect you, you don’t need to cut it out.
Can wearable tech really predict flares?
Yes-early data shows it can. FlareGuard AI, approved by the FDA in 2023, uses heart rate variability, sleep quality, and activity levels to predict flares 72 hours in advance with 76% accuracy. NIH research is even more advanced, predicting lupus flares 14 days ahead using blood biomarkers. These tools aren’t perfect yet, but they’re changing how we manage disease.
Should I take steroids at the first sign of a flare?
Only if your doctor has given you a plan. Steroids are powerful and fast-acting, but they carry risks: bone loss, weight gain, mood swings, and weakened immunity. If you’ve been told to use a short burst at flare onset, follow that plan. But don’t self-prescribe. Long-term steroid use leads to serious side effects. Work with your doctor to create a flare action plan.