Many people assume that if a herbal supplement is sold in a store or online, it’s safe. That’s a dangerous myth. The FDA doesn’t approve herbal products before they hit the market. Instead, it waits for harm to happen - then issues warnings. And those warnings often point to products that can cause serious harm if you’re also taking prescription meds.
What the FDA Actually Does (and Doesn’t Do)
The FDA regulates herbal supplements under the Dietary Supplement Health and Education Act (DSHEA) of 1994. That law lets companies sell products without proving they work or are safe. All they need to do is label them correctly and avoid making direct drug claims like “cures cancer.” But here’s the catch: many products slip through the cracks. Some contain hidden pharmaceuticals. Others are contaminated with heavy metals or bacteria. And nearly all of them can interact dangerously with medications you’re already taking.
Unlike prescription drugs - which go through 8 to 12 years of testing and cost over $2 billion to bring to market - herbal supplements enter the U.S. with zero pre-market safety review. The FDA only steps in after someone gets hurt. Between 2002 and 2023, the agency issued over 1,800 warning letters to supplement companies. Most of those were for products making false claims about treating diabetes, heart disease, or erectile dysfunction.
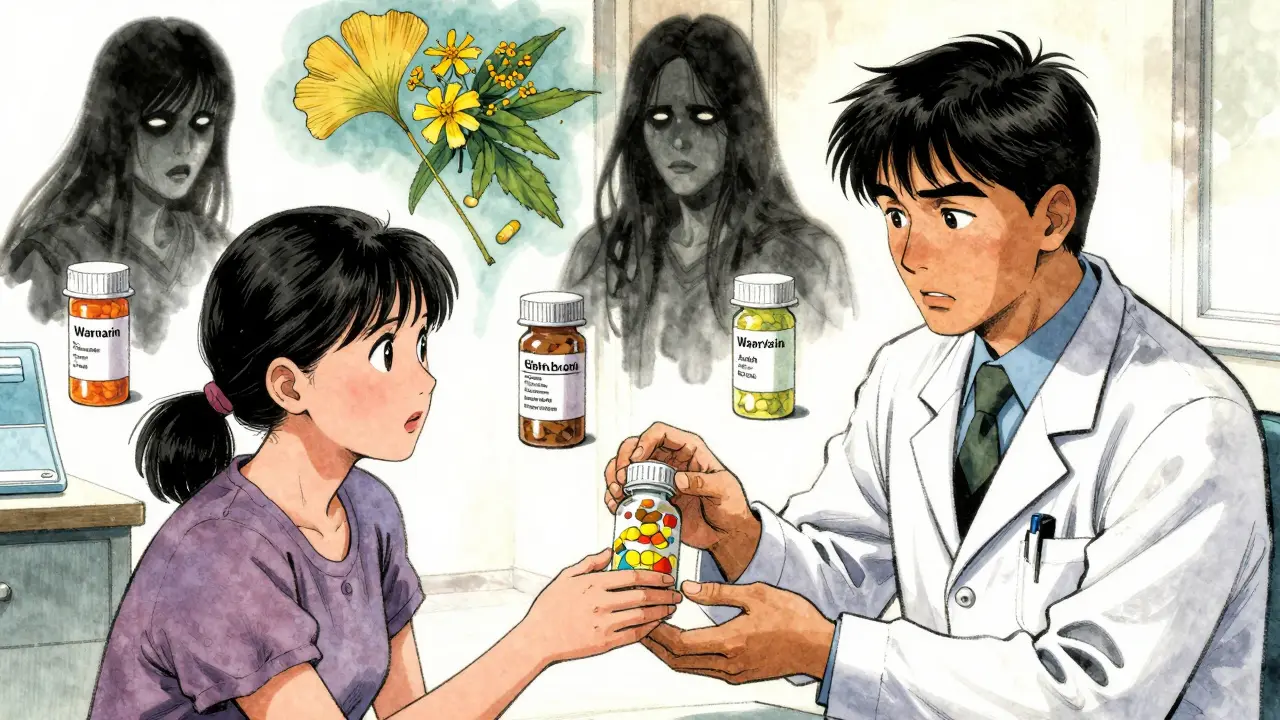
Herbal Products That Can Kill Your Meds
Some herbs don’t just sit quietly in your system. They actively interfere with how your body processes medications. Here are the top three that the FDA and medical experts warn about:
- St. John’s Wort: This popular herb for mild depression can slash the effectiveness of birth control pills, blood thinners like warfarin, antidepressants, and even HIV meds. One study found it reduced the concentration of cyclosporine - a drug used after organ transplants - by up to 60%. That’s not a side effect. That’s a life-threatening drop in drug levels.
- Ginkgo Biloba: Often taken for memory or circulation, ginkgo thins the blood. When combined with aspirin, ibuprofen, or warfarin, it can lead to uncontrolled bleeding. A 2021 case report in the Journal of Clinical Pharmacy and Therapeutics described a patient who bled internally after starting ginkgo without telling their doctor. They were on warfarin. The combination was deadly.
- Green Tea Extract: While drinking green tea is fine, concentrated extracts in pills have been linked to liver damage. The FDA has received over 100 reports of acute liver injury from these supplements since 2010. People who took them for weight loss were most affected. Some products contained high doses of EGCG, a compound that can overwhelm the liver when taken in pill form.
These aren’t rare cases. A 2018 study by Harvard Medical School found that nearly 800 supplements contained undeclared pharmaceuticals - and 41% had multiple hidden drugs. One “natural” weight loss product was found to contain sibutramine, a banned appetite suppressant linked to strokes and heart attacks. Another “male enhancement” pill had sildenafil (the active ingredient in Viagra) - but without dosage controls or warnings for people with heart conditions.
Why You’re Not Telling Your Doctor
Here’s the biggest problem: most people don’t tell their doctors they’re taking supplements. A 2022 survey of 1.5 million doctors found that 68% of patients never mention herbal products during appointments. Why? Many think supplements are “natural,” so they’re harmless. Others assume their doctor already knows. Some fear being judged.
But doctors need this info. If you’re on blood pressure meds and start taking hawthorn berry, your blood pressure could crash. If you’re on thyroid medication and take kelp supplements, your hormone levels can go haywire. A 2020 pilot program at Johns Hopkins Hospital showed that when doctors asked patients five simple questions - “Are you taking any supplements? What for? How much? How often? Any side effects?” - disclosure rates jumped from 32% to 78% in just six months.

How to Spot a Dangerous Supplement
You can’t trust labels. The FDA doesn’t test every product. But you can protect yourself with these checks:
- Look for USP, NSF, or ConsumerLab verification. These third-party seals mean the product was independently tested for what’s on the label - and what’s not. Verified products are 94% accurate in ingredient claims. Non-verified ones? Only 67%.
- Check the Latin name. If a label says “ginkgo,” it should also say Ginkgo biloba. If it doesn’t, it might not be the real herb - or it could be mixed with something else.
- Search the FDA’s warning letter database. Type the brand name into the FDA’s public database. If it’s been flagged, you’ll see the violation - like undeclared drugs or unsanitary manufacturing.
- Avoid products that promise quick fixes. “Lose 20 pounds in 2 weeks.” “Cure diabetes in 30 days.” “Instant erection.” These are red flags. Legitimate supplements don’t make drug-like claims.
Weight loss, sexual enhancement, and bodybuilding supplements are the most likely to be contaminated. The FDA has found illegal drugs in 42% of weight loss products, 29% of sexual enhancement products, and 18% of bodybuilding supplements. These are the categories that have led to hospitalizations - and deaths.
What Happens When You Don’t Disclose
Supplement interactions don’t always cause immediate harm. Sometimes, the damage builds up slowly. A patient taking statins for cholesterol might start taking red yeast rice - a natural statin - and end up with muscle breakdown. Another person on antidepressants might add 5-HTP for mood support, triggering serotonin syndrome - a rare but deadly condition.
The FDA’s MedWatch system collects adverse event reports, but only about 1% of incidents are reported. Most people don’t connect their symptoms to a supplement. They blame the flu. Or stress. Or aging. But when doctors finally find the link, it’s often too late.
One woman in her 50s took ashwagandha for stress. She didn’t tell her doctor she was on levothyroxine for hypothyroidism. Within weeks, her thyroid levels spiked. Her heart raced. She ended up in the ER. The ashwagandha had interfered with her thyroid meds. She didn’t know it could do that.

What You Can Do Right Now
You don’t need to stop all supplements. But you do need to be smart:
- Make a list. Write down every supplement, herb, and vitamin you take - including dosages and how often.
- Bring it to every appointment. Don’t wait for your doctor to ask. Hand them the list.
- Use the FDA’s Safety Reporting Portal. If you have a bad reaction, report it. It takes 10 minutes. Your report helps protect others.
- Download the NCCIH app. The National Center for Complementary and Integrative Health offers a free app with science-backed info on 1,200+ herbal products. It tells you what’s proven, what’s risky, and what interacts with meds.
- Choose verified products. Look for the USP Verified mark. It’s not perfect, but it’s the best safety net you’ve got.
The supplement industry is worth over $50 billion. And it’s growing fast. But safety hasn’t kept up. The FDA has only 45 staff members to oversee more than 30,000 companies. That’s one person for every 670 brands. You can’t rely on regulators. You have to protect yourself.
It’s Not About Avoiding Herbs - It’s About Using Them Wisely
Herbs have been used for thousands of years. Many have real benefits. But when you mix them with modern medicine, you’re playing with fire. The FDA’s warnings aren’t scare tactics. They’re emergency signals. If your doctor doesn’t know you’re taking something, they can’t help you if things go wrong.
Don’t assume natural means safe. Don’t assume your doctor knows. And don’t assume you’re the exception. Thousands of people have been hurt - and some have died - because they didn’t disclose what they were taking. Your health isn’t a secret. Tell your doctor. It could save your life.
Do herbal supplements need FDA approval before being sold?
No. Under the DSHEA law of 1994, herbal supplements don’t need FDA approval before being sold. Manufacturers only need to notify the FDA about new ingredients, but they don’t have to prove safety or effectiveness. The FDA can only act after a product is on the market and shown to be harmful.
Can herbal supplements interact with prescription medications?
Yes. Many herbal supplements interfere with how your body processes prescription drugs. St. John’s Wort can make birth control, antidepressants, and blood thinners less effective. Ginkgo biloba can increase bleeding risk when taken with aspirin or warfarin. Green tea extract can damage the liver, especially when combined with other liver-stressing medications.
Why don’t doctors always know about my supplements?
Most patients don’t tell their doctors because they assume supplements are harmless, or they’re afraid of being judged. But studies show that 68% of doctors encounter patients who hide supplement use. This creates serious risks - like dangerous drug interactions that could lead to hospitalization or death.
How can I tell if a supplement is safe?
Look for third-party verification seals like USP, NSF, or ConsumerLab. These mean the product was tested for what’s on the label and free of contaminants. Avoid products that promise quick fixes like “cure diabetes” or “instant weight loss.” Also, check the FDA’s warning letter database for your brand name. If it’s been flagged, walk away.
What should I do if I have a bad reaction to a supplement?
Stop taking it immediately and contact your doctor. Then, report the reaction to the FDA’s Safety Reporting Portal. Even if you’re not sure it was the supplement, your report helps the FDA track dangerous products. Between 2018 and 2022, over 14,000 adverse events were reported - but experts believe less than 1% of real incidents are reported.
For more information, use the National Center for Complementary and Integrative Health’s free mobile app. It has science-backed facts on over 1,200 herbal products - no hype, no ads, just what you need to know.
Man, I took that ginkgo stuff for ‘brain boost’ last year. Didn’t tell my doc I was on warfarin. Lucky I didn’t bleed out. Now I only buy USP-certified crap. Still think it’s a joke that the FDA lets this stuff fly under the radar.