What Exactly Is COPD?
COPD isn’t one disease-it’s a group of lung conditions that make it hard to breathe. The two main pieces are chronic bronchitis and emphysema. Even though they often show up together, they damage your lungs in completely different ways. If you or someone you know has COPD, knowing which part is dominant makes a real difference in treatment, daily life, and long-term outcomes.
Chronic Bronchitis: The Mucus Problem
Chronic bronchitis is defined by one clear sign: a cough that brings up mucus, lasting at least three months a year for two years straight. It’s not just a bad cold that won’t go away-it’s your airways swelling up and producing way too much mucus. The lining of your bronchial tubes thickens, and the mucus-making cells (goblet cells) multiply by 300% to 500%. That’s why people with this condition often clear 100 to 200 milliliters of mucus a day-enough to fill a small water bottle.
That thick mucus doesn’t just sit there. It clogs the airways, making it harder to get air in and out. People describe it as feeling like they’re breathing through a straw packed with glue. Many report spending 20 to 30 minutes every morning doing chest physiotherapy just to clear their lungs. Winter is especially rough-68% of patients have flare-ups during colder months, often triggered by viruses or pollution.
On the outside, you might see what’s called the “blue bloater” look: lips or fingernails with a bluish tint from low oxygen, swollen ankles from fluid buildup, and a tendency to tire easily even with light activity. Their oxygen levels often sit between 85% and 89%, which is dangerously low over time.
Emphysema: The Collapsed Air Sacs
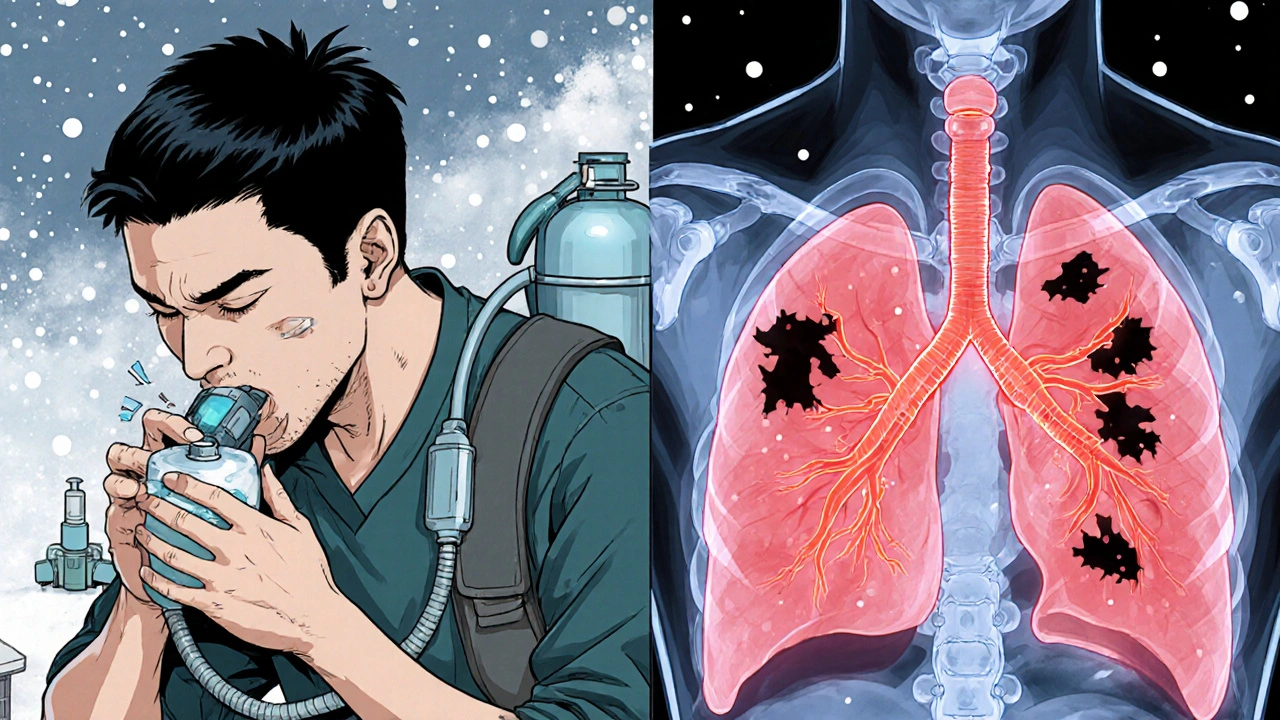
Emphysema doesn’t cause a cough or mucus. Instead, it quietly destroys the tiny air sacs in your lungs-called alveoli. These sacs are like little balloons that stretch and shrink to help you swap oxygen and carbon dioxide. In emphysema, the walls between them break down, turning many small sacs into a few giant, useless ones. You lose 30% to 50% of your lung’s natural springiness. That means your lungs can’t push air out properly, so air gets trapped.
People with emphysema don’t feel like they’re choking on mucus. They feel like they can’t get enough air-no matter how hard they breathe. This is called “air hunger.” Many can only speak in short bursts of five or six words before needing to stop and catch their breath. Over time, their chest shape changes. The rib cage expands outward, creating a “barrel chest.” Their breathing rate speeds up to 25 to 30 breaths per minute just to stay oxygenated.
They’re called “pink puffers” because their skin stays relatively pink-they’re working so hard to breathe that they push oxygen through, even if it’s inefficient. Their oxygen levels are often normal (92% to 95%) until late stages. But the damage is worse: their lung’s ability to transfer oxygen into the blood (DLCO) drops by 40% to 60%.
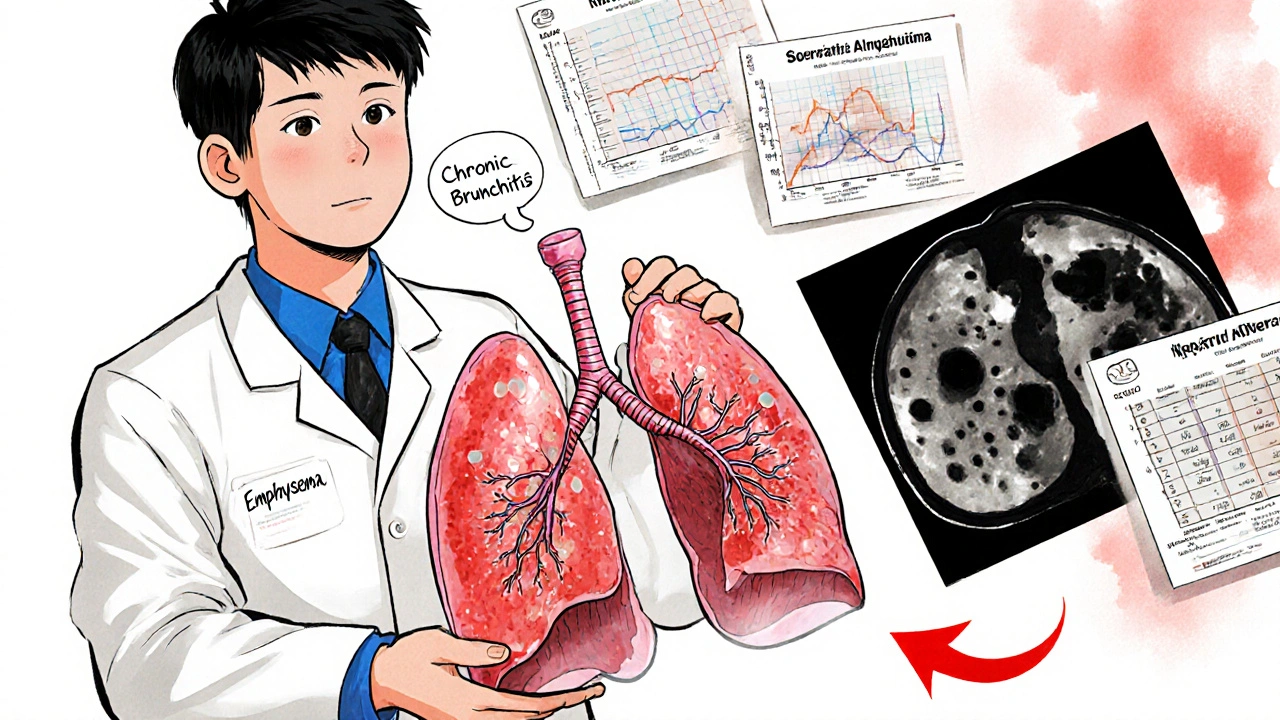
How Doctors Tell Them Apart
It’s not enough to just listen to symptoms. Doctors need tests to know what’s really going on. A simple spirometry test shows airflow blockage in both conditions-but that’s where the similarity ends.
- In chronic bronchitis, the FEV1/FVC ratio is low (under 70%), but the DLCO (diffusing capacity) stays normal or only slightly down.
- In emphysema, the DLCO is the key red flag-it drops below 60% of what’s expected for your age and size.
High-resolution CT scans show even clearer differences. Emphysema shows up as dark, patchy areas covering more than 15% of the lung-places where the tissue has collapsed. Chronic bronchitis shows thickened airway walls, with more than 60% of the airway cross-section taken up by swollen tissue.
There’s also the 6-minute walk test. People with emphysema usually drop their oxygen below 88% within the first two minutes. Those with chronic bronchitis stay oxygenated but stop walking because they’re too breathless.
Why It Matters: Treatment Isn’t One-Size-Fits-All
Here’s the big takeaway: treating COPD like it’s one disease leads to worse outcomes. A 2022 study showed patients who got care tailored to their specific type had 27% fewer hospital visits.
For chronic bronchitis, the goal is to thin and clear mucus. Mucolytics like carbocisteine cut flare-ups by 22%. Hypertonic saline nebulizers help loosen mucus-73% of users report easier clearing. Avoiding inhaled steroids is critical too-those with chronic bronchitis have a 40% higher risk of pneumonia from them. First-line treatment? Long-acting bronchodilators (LAMA/LABA combinations) that open the airways without the risks.
For emphysema, the focus is on saving lung function and removing trapped air. Lung volume reduction surgery or endobronchial valves can help. In the 2021 IMPACT trial, patients who got valves improved their walking distance by 35% in just six months. For the rare 1% to 2% with alpha-1 antitrypsin deficiency, weekly infusions of the missing protein can slow damage. New inhaled versions of this therapy, approved in 2023, show a 20% improvement in lung function within a year.
What Patients Actually Experience
Real people don’t fit neatly into textbook boxes, but their stories reveal the truth.
One Reddit user with emphysema said: “I can’t sing to my kids anymore. Even saying ‘I love you’ takes three breaths.” Another with chronic bronchitis described measuring her morning mucus in a cup-100 milliliters, every day, for eight years.
Emphysema patients often struggle with mobility. Even portable oxygen tanks feel like anchors. Chronic bronchitis patients battle daily routines: inhalers four to six times a day, chest percussion, humidifiers, and avoiding cold air.
But there’s hope. A 2022 European study found that using a special acoustic device to shake loose mucus reduced flare-ups by 32%. For emphysema, a new procedure called bronchoscopic thermal vapor ablation has a 78% success rate in improving breathing after two years.
The Bigger Picture
Most people with advanced COPD have features of both conditions-only about 15% have a pure form. But that doesn’t mean we should ignore the differences. Even if both are present, one usually dominates. Treating the dominant part first gives the biggest payoff.
Doctors are getting better at spotting this. Pulmonologists correctly identify the phenotype 78% of the time, but only 42% of primary care doctors do. That gap means many patients are getting the wrong meds-antibiotics when they need mucus thinners, or steroids when they’re at risk for pneumonia.
Research is moving fast. The NIH is tracking blood markers like eosinophils to predict who’ll respond to new biologic drugs. New medications like ensifentrine, designed specifically for chronic bronchitis, hit the market in 2023. And by 2026, a major study called SPIROMICS-2 will enroll 10,000 people to find better ways to personalize treatment.
What You Can Do Now
- If you have a long-term cough with mucus, get a spirometry test and ask for DLCO.
- If you’re breathless with little mucus, ask about CT scans and lung volume tests.
- Don’t assume all COPD meds are the same-your treatment should match your symptoms.
- Join a support group. The COPD Foundation has over 200 local chapters and online forums where people share what actually works.
- Track your symptoms: How many days a month do you cough? Do you feel better after clearing mucus? Do you get winded walking up one flight of stairs?
The future of COPD care isn’t about one pill or one surgery. It’s about matching the right treatment to the right lung problem. And that starts with knowing whether it’s the mucus-or the collapsed sacs-that’s holding you back.
Can you have chronic bronchitis without emphysema?
Yes. While many people with chronic bronchitis eventually develop some emphysema, especially if they smoke long-term, it’s possible to have chronic bronchitis as a standalone condition. It’s often seen in people exposed to heavy air pollution or occupational dusts who never smoked. The key is the persistent cough and mucus production over two years-not the lung destruction seen in emphysema.
Is emphysema worse than chronic bronchitis?
Neither is inherently “worse”-they just affect life differently. Emphysema causes severe shortness of breath and limits physical activity more quickly. Chronic bronchitis causes more frequent flare-ups, hospital visits, and nighttime disruptions. Emphysema patients often have better oxygen levels until late stages, while chronic bronchitis patients suffer from chronic low oxygen and heart strain. The real danger is when both are present and mismanaged.
Do I need a CT scan to diagnose COPD type?
Not always, but it’s the most accurate way to tell the difference. Spirometry confirms COPD, but a high-resolution CT scan shows exactly what’s damaged-whether it’s the air sacs (emphysema) or the airway walls (chronic bronchitis). If your symptoms don’t match your lung test results, or if you’re being considered for advanced treatments like lung valves, a CT scan is essential.
Can quitting smoking reverse either condition?
No, the damage from emphysema and chronic bronchitis can’t be undone. But quitting smoking is the single most effective thing you can do. It slows progression dramatically. People who quit after diagnosis live longer, have fewer flare-ups, and respond better to treatments. Even if you’ve smoked for 30 years, stopping now still adds years to your life.
What’s the best inhaler for chronic bronchitis vs. emphysema?
For chronic bronchitis, LAMA/LABA combos (like glycopyrrolate/formoterol) are preferred because they open airways without increasing pneumonia risk. Avoid inhaled steroids unless absolutely necessary. For emphysema, the same LAMA/LABA combos are first-line, but if you’re a “pink puffer” with very low lung function, your doctor may consider adding roflumilast (for inflammation) or exploring lung volume reduction options. Always base treatment on symptoms and test results-not labels.
What’s Next?
If you’re managing COPD, start by asking your doctor: “Which part is driving my symptoms-mucus or air trapping?” Then ask for a DLCO test and consider a CT scan if you’re not improving. Join a patient support group. Track your symptoms in a notebook. Small steps, guided by the right information, can lead to big improvements in how you live each day.
Okay but have you ever tried to explain to your mom why you can’t hug her without gasping like a fish on land? Emphysema ain’t just ‘bad lungs’-it’s your body screaming for mercy while your brain screams ‘just keep walking.’ I used to think breathing was automatic. Now I count every inhale like it’s my last damn dollar.
And don’t even get me started on mucus. My grandma used to say, ‘If you ain’t coughin’, you ain’t livin.’ Turns out she was wrong. You’re just drowning in your own body.
Also-yes, quitting smoking helps. But if you’re already in the thick of it? It’s not about guilt. It’s about getting the right tools. Not more steroids. Not more antibiotics. Just the damn science that actually works.