What Exactly Is a Corneal Ulcer?
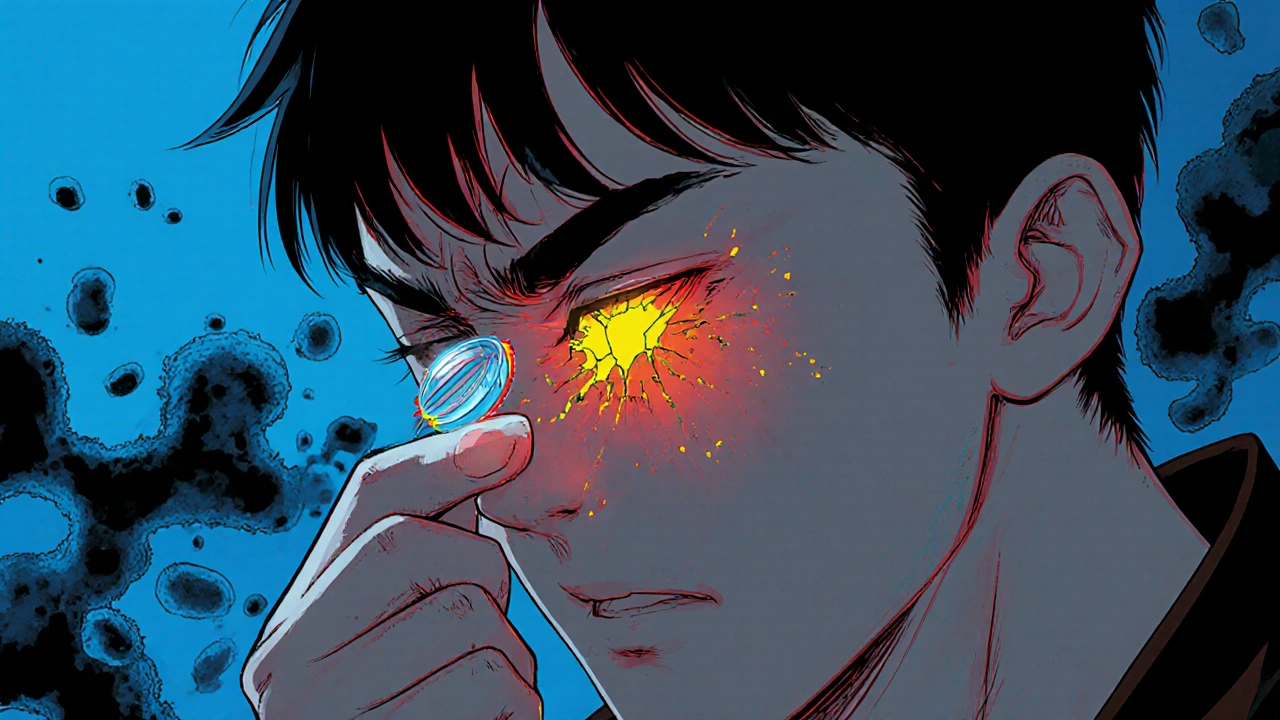
A corneal ulcer is an open sore on the clear front surface of your eye - the cornea. It’s not just a scratch. It’s tissue loss caused by infection, often from bacteria, fungi, or viruses that get trapped under your contact lens. Unlike a minor abrasion that heals on its own, a corneal ulcer eats away at the cornea. Left untreated, it can scar your vision permanently or even lead to blindness.
The risk isn’t theoretical. Over 85 million people worldwide wear contact lenses, and for some, this simple habit turns into a medical emergency. The FDA calls corneal ulcers one of the most serious hazards of contact lens use. And if you sleep in your lenses? Your risk jumps 100 times higher than someone who doesn’t wear contacts at all.
Why Contact Lenses Increase Your Risk
Contact lenses aren’t the problem - improper use is. Your cornea needs oxygen. When you wear lenses, especially overnight, you block that oxygen flow. That’s bad enough. But then you add dirt, bacteria, or fungi from your fingers, tap water, or dirty solution, and you’ve created the perfect storm.
Soft contact lenses, particularly extended-wear types, are the biggest offenders. They’re designed to be worn longer, but that convenience comes at a cost. A single night of sleeping in lenses can turn a harmless micro-scratch into a breeding ground for infection. Even a tiny tear in a lens can trap particles that scrape the cornea, giving germs an entry point.
Other factors make it worse:
- Wearing lenses while swimming, showering, or in hot tubs
- Using tap water to rinse or store lenses
- Not replacing lenses on schedule
- Using expired or non-recommended cleaning solutions
- Having dry eyes, blepharitis, or conditions like Bell’s palsy that prevent full eyelid closure
It’s not just about hygiene - it’s about biology. Your eye isn’t designed to live under a plastic film for 16 hours a day, let alone 24. The longer you push it, the higher the chance your cornea will break down.
Signs You Might Have a Corneal Ulcer
Don’t wait for it to get worse. These symptoms don’t come on slowly - they hit hard and fast:
- Severe eye pain, often described as a burning or gritty feeling
- Red, bloodshot eyes that won’t improve
- Blurry or hazy vision - like looking through a foggy window
- White or grayish spot on the cornea (you might not see it yourself, but your eye doctor will)
- Extreme sensitivity to light (photophobia)
- Excessive tearing or pus-like discharge
- Feeling like something’s stuck in your eye - even when there’s nothing there
If you’re wearing contacts and experience any of these, stop wearing them immediately. Don’t try to “wait it out.” Don’t use over-the-counter drops. This isn’t a red eye from tiredness. This is a medical emergency.

How Doctors Diagnose It
Your eye doctor won’t guess. They’ll test. The first step is usually fluorescein dye - a yellow-orange liquid that glows under blue light. Any damage to the cornea soaks up the dye and lights up like a map. That’s how they see the ulcer’s size and depth.
Next comes the slit-lamp exam. This high-powered microscope lets them zoom in on your cornea like a satellite image. They’ll look for signs of infection, swelling, or scarring.
If the ulcer is large or deep, they’ll take a scraping. A tiny tool gently removes a sample from the sore and sends it to the lab. This tells them if it’s bacterial, fungal, or viral. That’s critical because treatment changes completely based on the cause.
They’ll also check your vision with an eye chart and measure your cornea’s shape. These aren’t just routine checks - they’re survival tools.
How It’s Treated - Fast and Right
Time is vision. Every hour matters. Treatment starts immediately, even before test results come back.
For most bacterial ulcers - which make up the majority - doctors prescribe strong antibiotic eye drops, usually fluoroquinolones like moxifloxacin or gatifloxacin. You’ll need to use them every hour while awake for the first few days. That’s not a suggestion. That’s the protocol.
If it’s viral - often from herpes simplex - antiviral drops like acyclovir are used. Fungal ulcers? Those need specialized antifungal medications, sometimes even injected into the eye. These are rare but deadly if missed.
Here’s what you should never do: use steroid eye drops unless your doctor specifically prescribes them. Steroids reduce swelling, but they also suppress your immune system. In an infection, that’s like removing the guards from a castle. It can make things explode.
If the ulcer scars the cornea badly, vision won’t come back with drops alone. A corneal transplant may be the only option. It’s not common, but it’s life-changing when needed.
How to Prevent It - Simple Rules That Save Sight
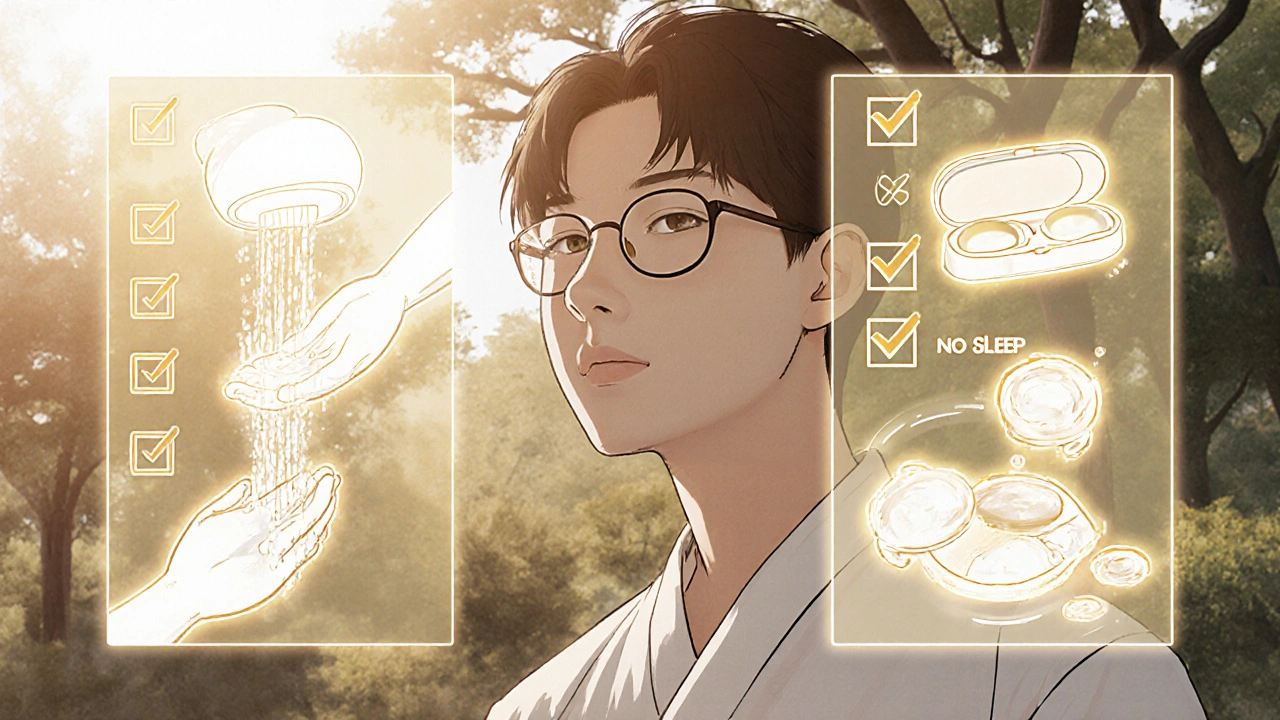
Prevention isn’t complicated. It’s just hard to stick to. Here’s what actually works:
- Never sleep in your lenses. Even if they’re labeled “extended wear,” your risk spikes 100 times. Take them out.
- Never expose lenses to water. No showers, no swimming, no rinsing with tap water. Water carries Acanthamoeba - a tough parasite that causes hard-to-treat infections.
- Wash your hands before touching lenses. Soap and water. Dry with a lint-free towel. Don’t skip this.
- Replace lenses on schedule. Daily disposables? Throw them out after one day. Monthly? Don’t wear them past 30 days, even if they feel fine.
- Use only the solution your doctor recommends. Never reuse old solution. Never top off the case. Clean the case daily, and replace it every three months.
- Give your eyes a break. Wear glasses at least one day a week. Let your cornea breathe.
These aren’t suggestions from a brochure. These are the rules that separate people who keep their vision from people who don’t.
When to Go to the Emergency Eye Clinic
If you’re wearing contacts and suddenly have severe pain, vision changes, or light sensitivity - go now. Don’t wait for your regular appointment. Don’t call your GP. Go straight to an eye specialist or emergency eye clinic.
Corneal ulcers don’t wait. They spread fast. In 48 hours, a small ulcer can grow, deepen, and threaten your central vision. That’s why doctors say: if you suspect a corneal ulcer, stop wearing lenses and seek care immediately.
There’s no home remedy. No eye rinse. No drop from the pharmacy that fixes this. Only professional care can stop the damage.
What Happens If You Ignore It
Ignoring a corneal ulcer is like ignoring a broken bone. At first, it might just hurt. Then it swells. Then it doesn’t heal. And then it breaks.
Scarring is permanent. Even after the infection clears, the scar tissue stays. That’s what causes blurry vision. In worse cases, the cornea can perforate - meaning it develops a hole. That’s when you risk losing the eye entirely.
People who delay care often end up needing transplants. Some never regain full vision. Others live with constant discomfort and light sensitivity for the rest of their lives.
This isn’t fearmongering. It’s fact. The FDA warns of blindness. The Cleveland Clinic calls it vision-threatening. And the data doesn’t lie: contact lens users are 10 times more likely to get a corneal ulcer than non-users. For those who sleep in lenses? The number is 100 times.
Looking Ahead - New Tech, Same Rules
There are new lenses with better oxygen flow. New cleaning solutions. Even antimicrobial coatings on some lenses. Diagnostic tools now use AI to analyze photos of ulcers faster than ever.
But here’s the truth: none of that replaces good habits. Technology can help, but it won’t fix bad behavior. The most effective tool you have is still your own discipline.
Every year, thousands of people lose vision because they thought, “It’s just a little red,” or “I’ll take them out tomorrow.” That tomorrow never comes - until it’s too late.
Dont sleep in lenses. Its that simple.