When your prescription comes back from the pharmacy with a different name than what your doctor wrote, it’s not a mistake-it’s generic substitution. This is when a pharmacist swaps your brand-name drug for a cheaper generic version. It’s legal, common, and often required by your insurance. But what happens when the switch doesn’t work for you? Or worse-when you didn’t even know it happened?
Generic drugs are not knockoffs. They contain the same active ingredient, strength, and dosage form as the brand-name version. The FDA requires them to be bioequivalent, meaning they work the same way in your body. In fact, 90% of all prescriptions filled in the U.S. are generics. But that doesn’t mean they’re all the same for every patient.
Why Insurance Pushes for Generics
Insurance companies don’t push generics because they want to save you money-they want to save themselves money. And honestly, they’re not wrong. A brand-name drug like Lipitor might cost $150 a month. The generic, atorvastatin? Around $10. That’s a 93% drop in cost. In 2023, generic drugs saved the U.S. healthcare system $373 billion. For insurers, that’s not a bonus-it’s a necessity.
Most private insurers, like Sun Life and Great West Life in Canada, have mandatory substitution policies. If your doctor writes a prescription for a brand-name drug, the insurer will only pay for the generic version. If you want the brand, you pay the difference out of pocket. Some even have policies that say, “Even if your doctor writes ‘do not substitute,’ we’ll still reimburse you for the generic price.”
It’s not just about price. Pharmacy benefit managers (PBMs)-companies like Express Scripts and CVS Caremark-control formularies. These are lists of drugs insurers will cover. If a brand-name drug isn’t on the list, it’s either blocked entirely or priced so high that patients can’t afford it. That’s how substitution becomes automatic.
When the Law Says No Substitution
But here’s the catch: the law doesn’t always let pharmacists switch your drug. In 19 U.S. states, pharmacists are required to substitute generics unless the doctor says otherwise. In 7 states and Washington, D.C., they must get your explicit permission first. In Texas, there are three clear rules: the generic must cost you less, you can’t refuse it, and your doctor must not have written “Brand Medically Necessary” on the prescription.
That phrase-“Brand Medically Necessary”-is your lifeline. If your doctor writes it on the prescription, the pharmacist can’t legally swap it out. No exceptions. No pressure from the insurer. No “we’ll cover the generic instead.”
Some patients need brand-name drugs because they react differently to the inactive ingredients in generics. Think fillers, dyes, or binders. These don’t affect how the drug works, but they can trigger allergies, stomach upset, or even changes in how the medicine is absorbed. A patient switching from Synthroid to generic levothyroxine might need three dose adjustments over six months because their body responds differently. That’s not rare. It’s documented.
What You Can Do If You’re Forced to Switch
If your insurance forces a switch and you feel worse, you have options. First, talk to your doctor. Not just to complain-to get documentation. Most insurers require a prior authorization request to cover a brand-name drug. That means your doctor has to submit proof that the generic didn’t work.
Blue Cross Blue Shield of Michigan, for example, requires doctors to show ICD-10 codes proving therapeutic failure. That could mean lab results showing your thyroid levels went out of range after switching, or your cholesterol spiked after switching from Lipitor. In their data, 78% of these requests get approved when the documentation is solid.
But here’s the problem: every insurer has different rules. Aetna wants three clinical criteria. UnitedHealthcare wants five. One requires a letter from your doctor. Another needs lab reports from the last three months. You can’t guess. You have to ask.
Call your insurer. Ask: “What do I need to submit to get approval for the brand-name version?” Write it down. Then give that list to your doctor. Don’t assume they know the exact paperwork. Most doctors don’t. They’re busy treating patients, not filling out insurance forms.
What Pharmacists Are Required to Tell You
Many people don’t realize they were switched until they get the bill. That’s because in 31 states, pharmacists are required to notify you when they substitute a drug. But that notice? It’s often buried on the receipt or in a small print slip. Some pharmacies even use a sticker on the bottle that says “Substituted for [Brand Name].”
If you’re not told, that’s a violation in those states. You have the right to know. And if you’re not told and something goes wrong, you can file a complaint with your state pharmacy board.
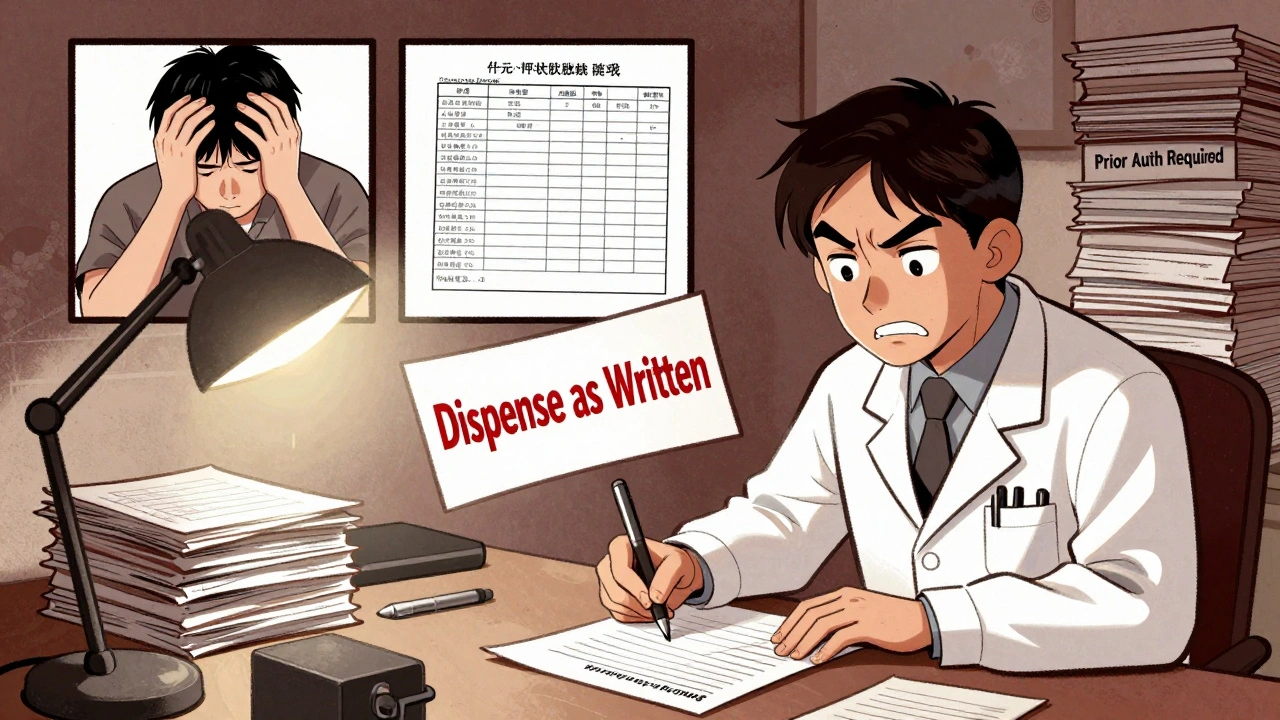
There’s also a big gap in communication between pharmacists and prescribers. In 37% of negative reviews on Drugs.com, patients reported being switched even when the prescription said “Dispense as Written.” That’s illegal in many places. If your doctor wrote it, and the pharmacist still swapped it, they broke the law. You can report it.
The Hidden Problem: Different Generics, Different Results
Not all generics are made the same. There are dozens of manufacturers making the same generic drug. One might use a different binder that slows absorption. Another might have a coating that dissolves faster. These differences don’t make the drug unsafe-but they can make it less effective for you.
Patients with epilepsy, thyroid conditions, or heart rhythm disorders are especially vulnerable. Even small changes in how a drug is absorbed can lead to seizures, unstable heart rates, or thyroid crashes. The FDA says approved generics are safe for everyone, including those on narrow therapeutic index drugs. But real-world experience tells a different story.
If you’ve had trouble with one generic, don’t assume the next one will be fine. Ask your pharmacist: “Which manufacturer is this from?” Then ask if you can stick with the same one each time. Many pharmacies will honor that request if you explain it’s for consistency.
What About Biologics and Complex Drugs?
Generics for pills? Easy. Generics for injections, inhalers, or biologics? Not so much. Biologics-like insulin, Humira, or Enbrel-are made from living cells. They’re complex. The FDA calls their generic versions “biosimilars,” not generics. And they’re not interchangeable unless proven to be.
As of November 2023, the U.S. had over 10,000 small-molecule generics. But only 38 biosimilars were approved. And in 38 states, you need extra consent before switching to a biosimilar. Some require the prescriber to be notified within five days. Others require you to sign a form.
If you’re on a biologic, don’t assume your insurance will let you switch. Check your plan’s formulary. Ask if your drug is listed as “interchangeable.” If it’s not, you’re protected from forced substitution.
How to Protect Yourself
Here’s a simple checklist to avoid surprise substitutions:
- Ask your doctor to write “Dispense as Written” or “Brand Medically Necessary” on your prescription-especially if you’ve had issues with generics before.
- When you pick up your prescription, check the label. Does it say the brand name? If not, ask: “Is this a generic? What manufacturer is it from?”
- Keep a log of how you feel after each refill. Note changes in energy, mood, side effects, or lab results.
- If you feel worse after a switch, don’t wait. Contact your doctor and your insurer immediately. Submit documentation for prior authorization.
- Know your state’s laws. Visit your state pharmacy board’s website to find out if you need consent before substitution.
Generic substitution saves money. But it shouldn’t cost you your health. You have rights. You have tools. And you don’t have to accept a substitution that doesn’t work for you.
What Happens If You Refuse a Generic?
If you refuse a generic and want the brand-name drug, you’ll pay the difference. That’s called “price differential.” Your insurer pays for the generic price. You pay the rest. So if the brand costs $150 and the generic is $10, you pay $140.
Some insurers offer a “brand exception” process. If your doctor documents medical necessity, they might cover the brand at the generic rate. But that’s rare. Most of the time, you’re paying extra.
Still, it’s better than getting sick because you were forced into a switch you didn’t agree to.
Can my pharmacist substitute my prescription without telling me?
In 31 U.S. states and Washington, D.C., pharmacists are legally required to notify you when they substitute a brand-name drug with a generic. If you weren’t told, that’s a violation. In states without notification laws, they still can’t substitute if your doctor wrote “Dispense as Written.” Always check your prescription label and ask if you’re unsure.
What if I feel worse after switching to a generic?
Track your symptoms and lab results. Contact your doctor and request a prior authorization for the brand-name drug. Insurers typically require proof of therapeutic failure-like abnormal blood tests or worsening symptoms. Submit this documentation. Many approvals are granted when the evidence is clear.
Are all generic drugs the same?
No. While all generics contain the same active ingredient, they can differ in inactive ingredients like fillers, dyes, or coatings. These can affect how the drug is absorbed, especially for people with sensitivities. If you’ve had a bad reaction to one generic, ask your pharmacist to stick with the same manufacturer each time.
Can my doctor stop my insurance from switching my drug?
Yes. If your doctor writes “Brand Medically Necessary” or “Dispense as Written” on your prescription, pharmacists are legally barred from substituting it in most states. This is your strongest protection. Make sure the wording is exact-some insurers reject vague phrases like “prefer brand.”
Do insurance companies ever cover brand-name drugs without extra cost?
Rarely. Most insurers require prior authorization with documented medical necessity. If approved, you may still pay a higher copay. Only in rare cases-like when no generic exists or when the generic is unavailable-will insurers cover the brand at the same cost as the generic. Always ask your insurer directly about their policy.
Final Thoughts
Generic substitution isn’t the enemy. It’s a tool. Used right, it saves billions and keeps care affordable. Used wrong, it can disrupt your health. The key isn’t to fight generics-it’s to control the process. Know your rights. Know your doctor’s role. Know your insurer’s rules. And never assume you’re being told the whole story.
If you’ve been switched without consent, if you’ve felt worse after a change, if your doctor warned you-but it happened anyway-you’re not alone. And you’re not powerless. Take action. Document everything. Speak up. Your health isn’t a cost-saving line item.

so i got switched from my brand name thyroid med to some generic last year and my heart started racing like i’d chugged 5 espressos. i went to my doc and they were like ‘it’s the same chemical’-nope. my body knows. now i pay $120 extra a month and i’m not sorry.