Every winter, shelves in pharmacies fill up with bottles labeled "cough relief," "congestion fighter," and "all-in-one cold cure." But how many of these actually help? And more importantly-do they make you safer, or just spend more money? The truth is, most over-the-counter cough and cold medicines don’t work the way we think they do. And for kids, some can be downright dangerous.
Why Most OTC Cold Medicines Don’t Work
The biggest culprit? Oral phenylephrine. It’s in almost every cold medicine you’ll find on the shelf-Sudafed PE, DayQuil, Robitussin, and dozens of others. You’ve probably bought it without thinking twice. But here’s the problem: oral phenylephrine doesn’t work as a decongestant at the doses sold over the counter.
In September 2023, the U.S. Food and Drug Administration (FDA) reviewed the science and concluded that 10 mg of oral phenylephrine-what’s in every tablet or liquid-has no better effect on nasal congestion than a sugar pill. Even the 25 mg dose (which isn’t sold to the public) only reduced congestion by about 28%. That’s not enough to make someone feel better. And yet, you’re still paying $10-$15 for something that does nothing.
It’s not just phenylephrine. Dextromethorphan, the cough suppressant in many syrups, has mixed results. Some studies show tiny benefits for adults. Others show no difference from placebo. Guaifenesin, the expectorant meant to thin mucus, has almost no solid evidence backing its use in adults or kids. And antihistamines? They don’t help with coughs at all-not even in kids with runny noses.
So what’s going on? These ingredients were approved decades ago based on weak data. Back then, regulators trusted manufacturers’ claims. Today, science has caught up. The FDA is now moving to remove phenylephrine from the list of approved OTC ingredients. That change could take effect by late 2025. When it does, you’ll see products reformulated-or disappear entirely.
Why Kids Are at Risk
If you’re a parent, this next part matters even more.
For children under 6, OTC cough and cold medicines aren’t just ineffective-they’re risky. The American Academy of Pediatrics has warned since 2007 that these products offer no real benefit for young kids, but can cause serious side effects: rapid heart rate, seizures, drowsiness, and even death.
Between 2000 and 2007, 20 children in the U.S. died after accidentally overdosing on OTC cold medicines. Thirteen of them were under two years old. Most of those deaths came from mixing multiple products-like giving a cough syrup and a fever reducer that both contained acetaminophen. Parents didn’t realize they were doubling the dose.
Even when used correctly, these medicines don’t make kids feel better faster. Studies show no difference in symptom duration or severity between kids who took cold medicine and those who didn’t. Yet, 73% of parents in one survey said they’d stopped giving OTC cold meds to kids under 6 after learning the risks. That’s a good sign.
The real solution? Simple, safe, and free. Humidified air. Saline nose drops. A bulb syringe to clear mucus. Plenty of fluids. And for kids over 12 months old? Honey.
One teaspoon of honey before bed has been shown in clinical trials to reduce nighttime coughing better than dextromethorphan. It’s natural, cheap, and doesn’t carry the risk of overdose. The only warning? Never give honey to babies under 12 months-it can cause infant botulism.

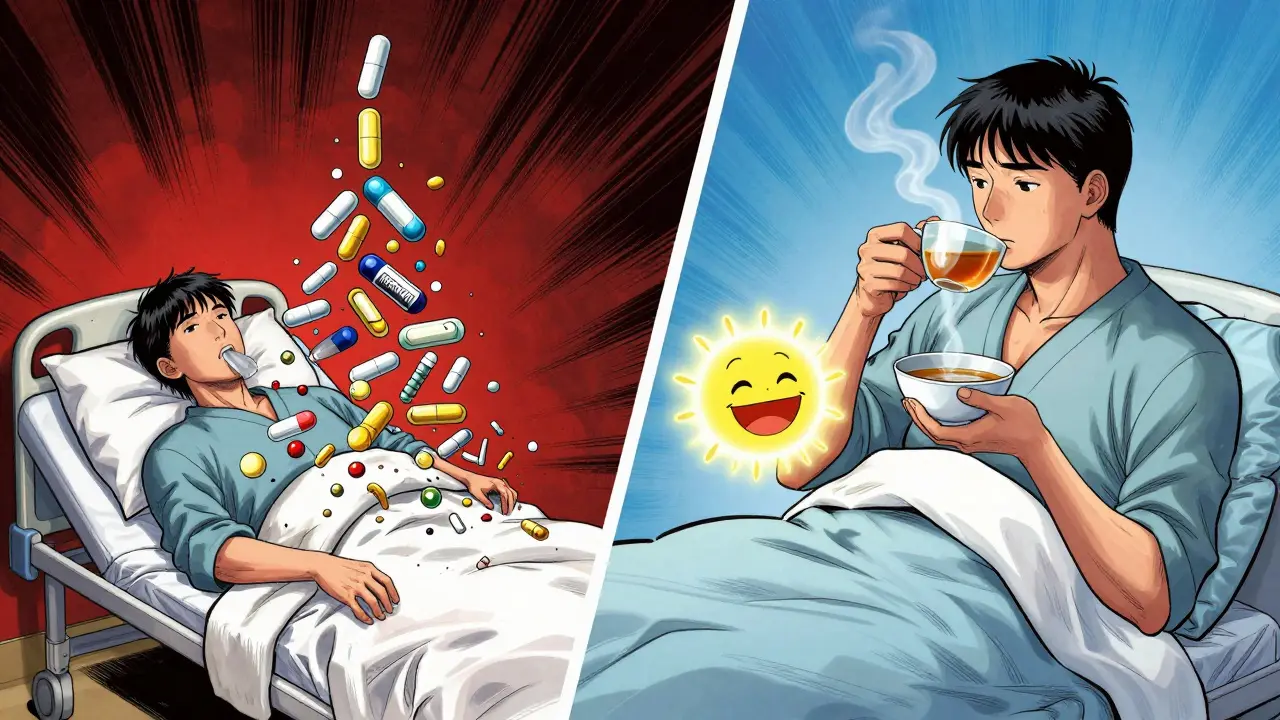
What Actually Works Instead
So if the pills and syrups don’t help, what does?
First, nasal sprays. Not the oral kind-intranasal decongestants. Oxymetazoline (found in Afrin) works quickly and directly on swollen nasal passages. It doesn’t get into your bloodstream like oral phenylephrine does. But here’s the catch: don’t use it for more than three days. After that, you risk rebound congestion-your nose gets worse when you stop.
Pseudoephedrine is another option. It’s the active ingredient in Sudafed (not Sudafed PE). It actually works. But you can’t just grab it off the shelf. You have to ask the pharmacist, show ID, and it’s kept behind the counter. Why? Because it’s used to make methamphetamine. The restrictions are real, but so is the effectiveness. If you’re an adult with bad congestion and you need relief, pseudoephedrine is still the best OTC option.
Steam and hydration matter more than you think. Breathing in warm, moist air from a shower or a bowl of hot water helps loosen mucus. Drinking water, broth, or tea keeps your throat moist and your body flushing out the virus. No pills needed.
And don’t underestimate rest. Your immune system doesn’t need chemicals to fight a cold-it needs sleep. Most colds last 7-10 days. No medicine changes that timeline. All it does is make you feel a little more comfortable while your body does the work.
Reading Labels: How to Avoid Dangerous Mistakes
Here’s where most people go wrong. You’ve got a stuffy nose, a sore throat, and a headache. So you grab a bottle that says "Full-Spectrum Cold Relief." It has acetaminophen for pain, dextromethorphan for cough, phenylephrine for congestion, and chlorpheniramine for runny nose.
Now you also grab a nighttime sleep aid because you can’t rest. It has diphenhydramine and acetaminophen. Suddenly, you’re taking two sources of acetaminophen. Too much can cause liver failure.
That’s why you must read the Drug Facts label. Look for the "Active Ingredients" section. Don’t assume different brands have different formulas. Many are identical under different names.
Rule of thumb: Never take two medicines with the same active ingredient. If you’re using a multi-symptom product, make sure you’re not doubling up on anything. And if you’re unsure, ask a pharmacist. They’re trained to catch these mistakes.
What’s Coming Next
The market is changing fast. With phenylephrine set to be removed from OTC products by 2025, companies are scrambling. Some will reformulate with pseudoephedrine (though that means stricter sales rules). Others will switch to saline sprays, honey-based syrups, or even menthol lozenges.
Consumer behavior is shifting too. A 2023 Harris Poll found that 63% of U.S. adults would switch to alternative remedies after learning phenylephrine doesn’t work. Sales of honey-based cough syrups and saline nasal rinses are growing at over 12% per year. People are realizing they don’t need a chemical fix for a viral infection.
And that’s the real lesson here. Colds are caused by viruses. No pill can kill them. The best you can do is manage symptoms while your body heals. That’s not a failure of medicine-it’s how the human body works.
What to Do Right Now
Here’s what you can do today, no matter your age:
- Check your medicine cabinet. If you have anything with "phenylephrine" on the label, you’re not getting any benefit. Consider replacing it.
- If you’re an adult with bad congestion, ask your pharmacist for pseudoephedrine. Show your ID. It’s worth it.
- If you have a child under 6, don’t give them OTC cough or cold medicine. Use saline drops, a humidifier, and honey (if they’re over 12 months).
- Drink water. Sleep. Breathe steam. These are your real remedies.
- Never mix cold medicines. Always check the active ingredients.
It’s easy to feel like you need something strong to beat a cold. But the truth is, the best medicine you have is already inside you. All you need to do is give your body the space and care to do its job.

Why do we keep paying for placebo pills? I bought a bottle of DayQuil last month and felt exactly the same after 8 hours as I did before. Zero improvement. Just a fancy sugar pill with a fancy label.
And yet, I still bought it. Because marketing is powerful and I’m weak.