Every year, thousands of people in hospitals and pharmacies around the world get the wrong medicine-not because someone was careless, but because two drugs look or sound almost exactly the same. And the worst part? Most of these mix-ups involve generic drugs.
Take hydralazine and hydroxyzine. One lowers blood pressure. The other treats anxiety and allergies. Both come in small white capsules. Both are prescribed in 10 mg doses. If a pharmacist grabs the wrong bottle-or a nurse hears "hydroxyzine" over a crackly intercom and writes down "hydralazine"-the result can be dangerous. A patient with high blood pressure could end up with a drug that does nothing for their heart, while their anxiety spikes. This isn’t hypothetical. It’s happened. And it happens more often than you think.
What Are Look-Alike, Sound-Alike (LASA) Drugs?
Look-alike, sound-alike (LASA) drugs are medications with names or packaging so similar that they can be confused during prescribing, dispensing, or giving them to patients. This isn’t just about spelling. It’s about how they look on the shelf, how they sound when spoken, and even how the bottle feels in your hand.
Look-alike errors happen when two drugs have similar shapes, colors, or label designs. For example, one generic version of a blood thinner might look almost identical to a generic diabetes pill-same size, same color, same font. Sound-alike errors happen when names rhyme or start with the same syllables. Think albuterol and atenolol. One opens airways for asthma. The other slows your heart for high blood pressure. Say them out loud. They’re almost twins.
Generics make this worse. When a brand-name drug loses its patent, dozens of companies start making the same medicine under different names. Each one uses slightly different packaging. Some use red caps. Others use blue. Some print the name in bold. Others in italics. No standard. No consistency. So now, instead of one confusing pair, you’ve got five versions of the same drug-each looking a little different-mixed in with other generics that have similar names.
Why Generics Are the Biggest Problem
Generic drugs are cheaper. That’s good. But the system that lets them be made by multiple companies also makes them harder to track. A hospital might buy generic metoprolol from three different manufacturers. One has a green label. One has a white label. One has a logo on the bottom. The pharmacy might stock them side by side. If a nurse is tired, rushed, or distracted-say, during a night shift-they might grab the wrong one.
And it’s not just the name. The pills themselves can look alike. A 5 mg tablet of one drug might be white and round. So is a 5 mg tablet of another. Same size. Same imprint. Same coating. Even the bottle caps might be the same color. In a busy ER, with ten patients waiting and lights flashing, that’s a recipe for disaster.
According to the World Health Organization, about 25% of all medication errors are caused by LASA drugs. And of those, more than half involve generic versions. The Institute for Safe Medication Practices (ISMP) tracks nearly 1,000 high-risk pairs. Some of the most dangerous? Valtrex and Valcyte. Both start with "Val-". Both are used in transplant patients. One treats herpes. The other treats a deadly CMV infection. Mix them up, and you could be giving someone a drug that does nothing against the virus they’re fighting.
Where Do These Errors Happen?
These mistakes don’t just happen in pharmacies. They happen everywhere.
- Prescribing: A doctor types "hydroxyzine" but the computer auto-fills "hydralazine" because they look similar on the screen.
- Dispensing: A pharmacist reaches for the bottle labeled "clonidine" but grabs "clonazepam"-same first four letters, same shelf.
- Administration: A nurse hears "dopamine" over the phone and writes down "dobutamine". Both are IV drugs used in ICUs. One boosts blood pressure. The other increases heart output. Give the wrong one, and the patient’s heart could stop.
A 2022 study in the American Journal of Nursing found that 78% of pharmacists had encountered a LASA error at least once a month. One in three said they’d had a near-miss-where they caught it just in time-every week.
And it’s not just adults. Children are especially vulnerable. A child given the wrong dose of a LASA drug can suffer brain damage, organ failure, or death. Even a tiny mistake-like confusing fluoxetine with fluvoxamine-can change a treatment plan completely.
What’s Being Done to Stop It?
People have been trying to fix this for years. And some things actually work.
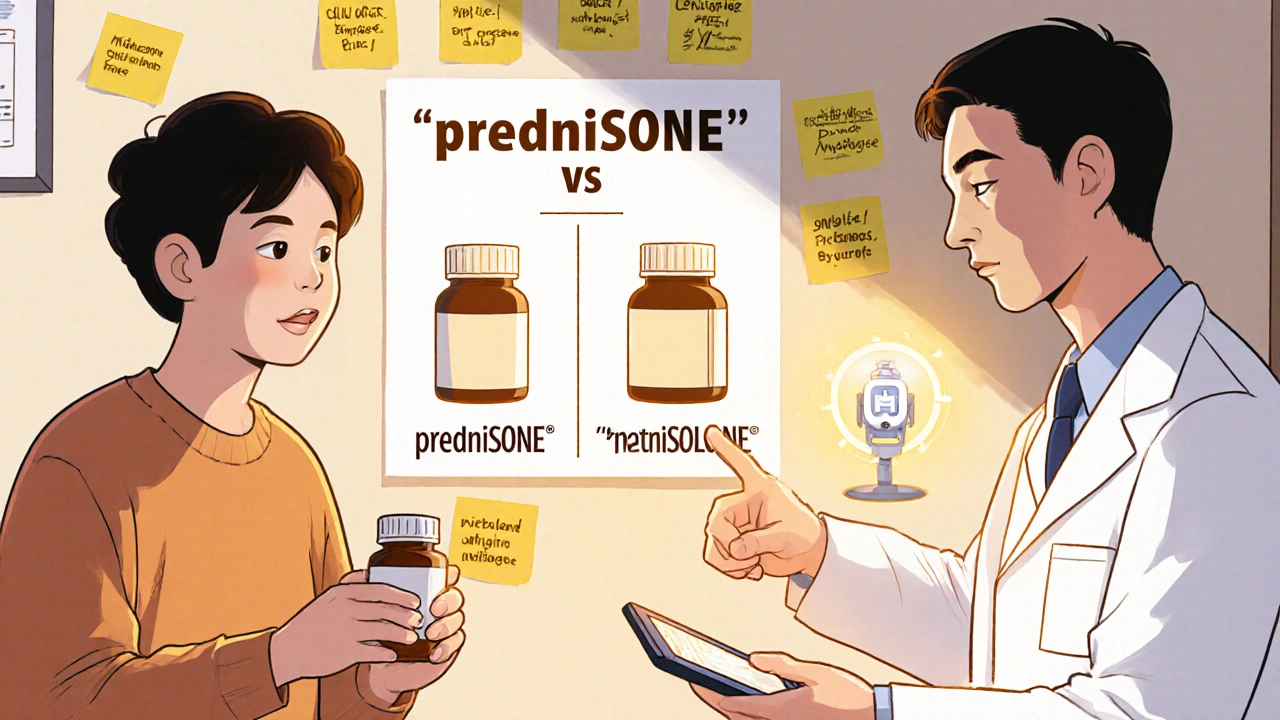
Tall man lettering is one of the most effective tools. Instead of writing "prednisone" and "prednisolone", hospitals now write "predniSONE" and "predniSOLONE". The capital letters highlight the difference. A 2020 study across 12 hospitals showed this simple change cut LASA errors by 67%.
Physical separation is another big one. Hospitals now keep high-risk LASA drugs on different shelves. One side of the pharmacy for blood pressure meds. Another for anxiety drugs. No more side-by-side bottles that look like twins.
Barcode scanning helps too. When a nurse scans a patient’s wristband and then the drug, the system checks: "Is this the right drug for this patient?" If it’s a LASA pair, it flashes a warning. One hospital system saw a 45% drop in errors after adding this.
And now, artificial intelligence is stepping in. New systems embedded in electronic health records can spot when a doctor types "atenolol" but meant "albuterol". They flag it. They suggest the correct drug. In a 6-month trial across three hospitals, AI caught 98.7% of potential LASA errors-and only gave a false alarm 1.3% of the time.
What’s Still Not Working
But here’s the problem: not everyone is using these tools.
In the U.S., the FDA rejected 34 drug names in 2021 because they were too similar to existing ones. That’s progress. But in other countries, there’s no such review. Generic manufacturers don’t have to change their packaging to stand out. No rules. No standards.
Even in hospitals that have barcode scanners and AI alerts, staff sometimes turn them off. Too many alerts. Too many false alarms. People get used to ignoring them. That’s called "alert fatigue". And it’s deadly.
And what about small clinics? Rural pharmacies? Nursing homes? They don’t have the budget for fancy AI systems. They rely on printed lists and memory. And when a pharmacist is working alone at 2 a.m., memory isn’t enough.
What You Can Do
You don’t have to be a doctor or a pharmacist to help prevent these errors.
- Know your meds. If you’re prescribed a generic drug, ask: "What is it for?" and "What does it look like?" Write it down. Keep a list.
- Check the label. When you pick up a prescription, compare the pill to the last one you got. Is the color different? The shape? The imprint? If it looks off, ask.
- Speak up. If a nurse says, "I’m giving you hydralazine," and you were told you were getting hydroxyzine-say something. Don’t assume they know better.
- Use one pharmacy. If you use the same pharmacy for all your meds, they’ll catch inconsistencies. They’ll know your history.
And if you’re a caregiver for an elderly parent or someone with multiple prescriptions? Make a simple chart. Name. Purpose. Color. Shape. Dose. Keep it in your wallet. Show it to every provider.
The Bigger Picture
Medication errors cost the global health system $42 billion a year. LASA errors are a big chunk of that. And they’re preventable.
The real problem isn’t that people make mistakes. It’s that we treat them like individual failures. A nurse grabs the wrong bottle? Blame the nurse. A doctor types the wrong name? Blame the doctor. But the system let it happen. The labels were too similar. The bottles were too close. The computer didn’t warn them. The training was rushed.
What we need isn’t more blame. It’s better design. Standardized packaging. Clearer names. Technology that works. And a culture where every person-patient, nurse, pharmacist, doctor-feels safe speaking up.
The World Health Organization’s "Medication Without Harm" campaign wants to cut severe medication errors by 50% by 2025. It’s ambitious. But possible. If we stop treating LASA errors as accidents and start treating them as system failures, we can fix them.
Because no one should die because two pills look too much alike.
What are some common look-alike, sound-alike drug pairs?
Common pairs include hydralazine/hydroxyzine, albuterol/atenolol, clonidine/clonazepam, dopamine/dobutamine, and Valtrex/Valcyte. These drugs have similar spellings, sounds, or packaging, making them easy to confuse. For example, hydralazine is for high blood pressure, while hydroxyzine treats anxiety-mixing them can lead to dangerous side effects.
Why are generic drugs more likely to cause LASA errors?
Generic drugs are made by multiple manufacturers, each using different packaging, colors, and label designs. Unlike brand-name drugs, which have consistent appearance, generics vary widely. This inconsistency makes it harder to tell similar-sounding or similar-looking drugs apart, especially when they’re stored next to each other in pharmacies or hospitals.
How effective is tall man lettering in preventing errors?
Tall man lettering-where key letters are capitalized to highlight differences (like predniSONE vs. predniSOLONE)-has been shown to reduce LASA errors by up to 67% in hospital settings. It’s a simple, low-cost method that makes visual similarities obvious, helping staff catch mistakes before they happen.
Can technology really stop these errors?
Yes. AI-powered clinical decision support systems embedded in electronic health records can flag potential LASA errors with 98.7% accuracy and only 1.3% false alarms. Barcode scanning and automated alerts also reduce errors by 40-50% in hospitals that use them consistently. But these tools only work if staff are trained and don’t disable them due to alert fatigue.
What should I do if I think I’ve been given the wrong generic medication?
Don’t take it. Compare the pill to your previous prescription-check the color, shape, size, and imprint. Ask the pharmacist: "Is this the same medication I got last time?" If something feels off, speak up. You have the right to know what you’re taking. If you’re unsure, call your doctor before taking it.
Are there any global standards for generic drug packaging?
No, there are no universal standards. The U.S. FDA and European Medicines Agency have guidelines and review new drug names for similarity, but they don’t regulate packaging design for generics. This means two identical generic drugs from different manufacturers can look completely different, increasing confusion. Advocates are pushing for global packaging standards, but progress has been slow.
What Comes Next?
The future of medication safety isn’t just about better tech-it’s about better thinking. We need to stop accepting LASA errors as "part of the job." They’re not. They’re preventable. Every hospital, every pharmacy, every clinic should have a list of high-risk pairs posted where staff can see them. Every patient should be encouraged to ask questions. Every drug name should be reviewed before it hits the market.
And if you’re taking a generic drug? Keep a picture of your pill on your phone. Write down what it’s for. Ask for the manufacturer’s name. Small steps. Big impact.
Medication safety isn’t just for doctors. It’s for all of us.
These LASA errors are a goddamn epidemic disguised as bureaucracy. Pills look like M&Ms and we act surprised when people die? We’re not fixing systems-we’re just blaming nurses while the pharma giants profit.