Diabetic ketoacidosis, or DKA, isn’t just a scary term-it’s a medical emergency that can turn deadly in hours. It happens when your body doesn’t have enough insulin to use sugar for energy, so it starts breaking down fat instead. That process floods your blood with acidic ketones, throwing your whole system out of balance. You don’t need to be a diabetic expert to recognize the signs. If you or someone you know has type 1 diabetes-or even type 2 and is skipping insulin-you need to know what to look for before it’s too late.
What DKA Looks Like: The Warning Signs
The early signs of DKA are easy to miss because they look like a bad flu or stomach bug. You feel thirsty all the time-not just a little, but so bad you’re drinking four to six liters of water a day. You’re peeing constantly, sometimes more than three liters in 24 hours. Your mouth feels like cotton. These aren’t just inconveniences; they’re your body screaming for help.Within 12 to 24 hours, things get worse. Nausea hits hard. Vomiting starts. You might have sharp abdominal pain that feels like appendicitis. Fatigue isn’t just being tired-it’s being too weak to get out of bed. Grip strength drops by 30-40%. You can’t hold a coffee cup steady. That’s not normal fatigue. That’s your muscles breaking down.
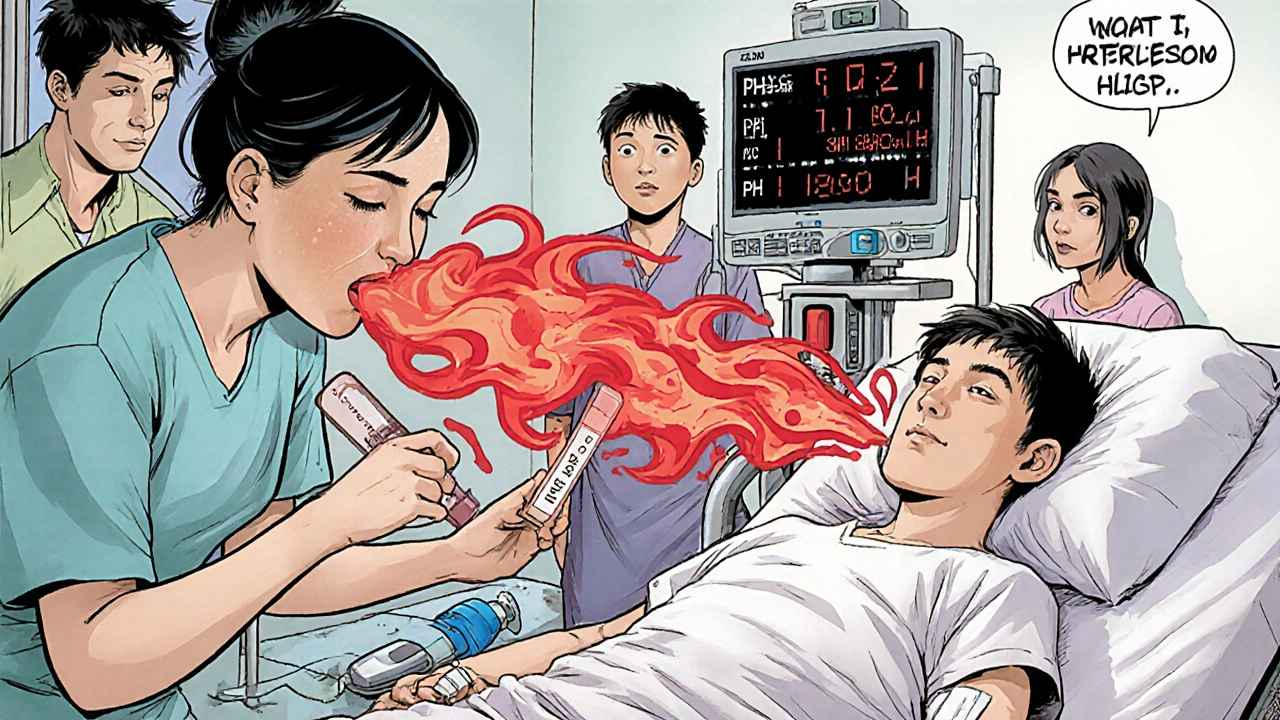
Then come the red flags that mean you need to go to the hospital right now. You start breathing fast and deep-Kussmaul respirations-like you’re trying to blow out a fire. Your breath smells sweet, like nail polish remover or rotten apples. That’s acetone, a ketone your body is dumping. You feel confused. Disoriented. Maybe even drowsy. If you’re slurring words or can’t focus, you’re in danger.
Doctors diagnose DKA with three key numbers: blood sugar over 250 mg/dL, blood pH below 7.3, and ketones above 3 mmol/L. But here’s something most people don’t know: about 10% of DKA cases happen with blood sugar under 250 mg/dL. This is called euglycemic DKA. It’s more common in people taking SGLT2 inhibitors (like Farxiga or Jardiance), and it’s easy to miss because glucose levels don’t scream danger. If you’re on one of these drugs and feel sick, check your ketones-even if your glucose looks normal.
Why DKA Happens: Triggers You Can’t Ignore
DKA doesn’t come out of nowhere. It’s usually triggered by something preventable. In half of all cases, it’s an infection-a cold, the flu, a urinary tract infection. Your body needs more insulin when you’re sick, but if you’re not adjusting your dose, your blood sugar spikes and ketones rise.One in three cases happen because insulin was skipped. Maybe you ran out. Maybe you couldn’t afford it. In the U.S., the average monthly cost of insulin is $374. People ration it. They skip doses. They wait too long to refill. That’s not laziness-it’s a system failure. And it’s deadly.
One in five cases are the first sign of undiagnosed type 1 diabetes. Kids show up at the ER vomiting and lethargic, and the doctors think it’s gastroenteritis. By the time they test for ketones, it’s too late. That’s why every child who comes in with unexplained vomiting and fatigue should get a blood sugar test. It takes 30 seconds. It could save their life.
Insulin pump users aren’t safe either. About 35% of pump-related DKA cases happen because the infusion set got clogged or disconnected. If you’re sick and your pump is beeping or your glucose is rising fast, switch to injections. Don’t wait.
What Happens in the Hospital
Once you’re admitted, time becomes your enemy. The longer you wait, the higher your risk of death. Every hour without fluids and insulin increases mortality risk by 15%. That’s why emergency rooms now use point-of-care ketone meters for anyone with blood sugar over 250 mg/dL. It’s fast. It’s accurate. It cuts missed diagnoses by 37%.First, you get fluids. You’re given 1 to 1.5 liters of salt water (0.9% sodium chloride) in the first hour. That’s not just hydration-it’s flushing out the acid. Then, you get insulin. Not a shot. Not pills. Continuous IV insulin at 0.1 unit per kg per hour. Your blood sugar should drop by 50 to 75 mg/dL per hour. Too fast? You risk brain swelling. Too slow? The acid keeps building.
Electrolytes are just as critical. Even if your blood potassium looks normal, your body is completely depleted. You’ll get 20 to 30 mEq of potassium per hour. Without it, your heart can stop.
Bicarbonate? Rarely used. Only if your blood pH drops below 6.9. Most hospitals still give it out of habit, but it doesn’t help. In fact, it can make things worse. The guidelines changed years ago. If your hospital is still giving bicarbonate, ask why.
You’ll be monitored hourly: glucose, ketones, electrolytes. Your stay averages 2.5 to 4 days. But here’s the kicker: if your pH is above 7.0 when you arrive, you’ll likely go home in two days. If it’s below 7.0, you’re looking at four. That’s why early action matters so much.

What Recovery Looks Like
You’re not out of the woods just because your glucose is normal. Treatment continues until three things are stable: ketones under 0.6 mmol/L, bicarbonate above 18 mmol/L, and pH above 7.3 on two consecutive checks. If you’re discharged too early, 12% of people end up back in the hospital within 72 hours.Once you’re stable, you’ll switch back to insulin injections or your pump. You’ll get education on sick-day rules: check ketones every 4-6 hours when glucose is over 240 mg/dL. Never skip insulin when you’re sick. Always have a backup plan.
Technology is changing the game. People using continuous glucose monitors (CGMs) like Dexcom G7 reduce DKA by 76%. Why? Because they get alerts when ketones start rising-even before glucose spikes. One user said, “My CGM beeped at 3 a.m. I checked ketones. I called my doctor. I avoided the ER.” That’s the future.
What You Can Do Today
If you have diabetes, make a plan. Keep ketone strips or a blood ketone meter at home. Know your trigger numbers. If your glucose is over 240 mg/dL and you feel off, test your ketones. Moderate or large ketones? Go to the ER. Don’t wait. Don’t call your doctor first. Go.If you’re caring for someone with diabetes, learn the signs. Don’t assume they’re just “not feeling well.” Vomiting, confusion, fruity breath-those aren’t normal. Call 911.
If you’re struggling to afford insulin, talk to your provider. There are patient assistance programs. Generic insulin is now available for under $25 a vial. You don’t have to choose between food and life-saving medication.
DKA is preventable. It’s treatable. But only if you act fast. The difference between a hospital stay and a death sentence is often just a few hours.
Can you have DKA with normal blood sugar?
Yes. About 10% of DKA cases happen with blood glucose under 250 mg/dL. This is called euglycemic DKA. It’s more common in people using SGLT2 inhibitors like Farxiga or Jardiance, or during fasting or illness. If you’re on one of these medications and feel sick, check your ketones-even if your glucose looks normal.
How long does it take for DKA to become life-threatening?
DKA can progress from mild symptoms to coma or death in as little as 24 hours. The risk of death increases by 15% for every hour treatment is delayed. Early signs like vomiting and fatigue can escalate quickly, especially in children or older adults. Don’t wait for confusion or unconsciousness to act.
Can insulin pumps cause DKA?
Yes. About 35% of DKA cases involving insulin pumps are caused by infusion set failures-clogs, disconnections, or air bubbles. During illness, your body needs more insulin, and a blocked set can’t deliver it. If your glucose is rising fast and you’re sick, switch to injections immediately. Always have a backup.
Is DKA more dangerous for children?
Yes. Children are at higher risk of cerebral edema-a dangerous brain swelling-that occurs in 0.5% to 1% of pediatric DKA cases and kills 21% to 24% of those affected. It’s linked to overly rapid fluid replacement or bicarbonate use. Hospitals now follow strict fluid protocols to prevent this. Parents should never delay care if their child is vomiting, lethargic, or breathing fast.
Can DKA happen in type 2 diabetes?
Yes. While most cases occur in type 1 diabetes, DKA can happen in type 2, especially during severe illness, infection, or when insulin is stopped. It’s more common in people with latent autoimmune diabetes (LADA) or those taking SGLT2 inhibitors. Never assume type 2 diabetes is “mild” or “safe.”
How can I prevent DKA?
Test your ketones when your blood sugar is over 240 mg/dL, especially if you’re sick, stressed, or not eating. Never skip insulin, even if you’re not eating. Have a sick-day plan with your doctor. Use a CGM with ketone alerts if possible. Keep emergency insulin and ketone strips on hand. If you can’t afford insulin, ask about patient assistance programs-your life depends on it.
Why do some hospitals still give bicarbonate for DKA?
Some hospitals still use bicarbonate out of habit, even though guidelines from the ADA and ISPAD say it’s only needed if pH is below 6.9. Studies show it doesn’t improve outcomes and can cause harm-like low potassium or brain swelling. If your hospital gives it routinely, ask if they follow current international standards.
What’s the most common mistake people make with DKA?
Waiting. Most people wait 6 hours or more after symptoms start before seeking help. They think it’s the flu, food poisoning, or stress. But DKA doesn’t wait. The average patient who delays care is 3 times more likely to need ICU admission. Recognizing the signs early saves lives.

Just read this after my cousin got hospitalized for DKA last month. I had no idea euglycemic DKA was a thing. We thought her glucose was fine so we waited a day. Big mistake. Now I keep ketone strips in the house. Everyone with diabetes should too.