Smoking and Alcohol Co-consumption is a public‑health phenomenon where individuals regularly use cigarettes and drink alcoholic beverages in the same setting. This dual habit drives far‑greater disease rates than either habit alone, creating a perfect storm for cancer, heart disease, and addiction.
Quick Takeaways
- Smoking and drinking together increase cancer risk by up to 5‑fold compared with single use.
- Both substances share dopamine pathways, making cravings mutually reinforcing.
- Combined exposure accelerates cardiovascular damage and liver injury.
- Public‑health policies that target one habit often miss the synergistic effect.
- Dual‑treatment programs that address both nicotine and alcohol dependence achieve the highest quit rates.
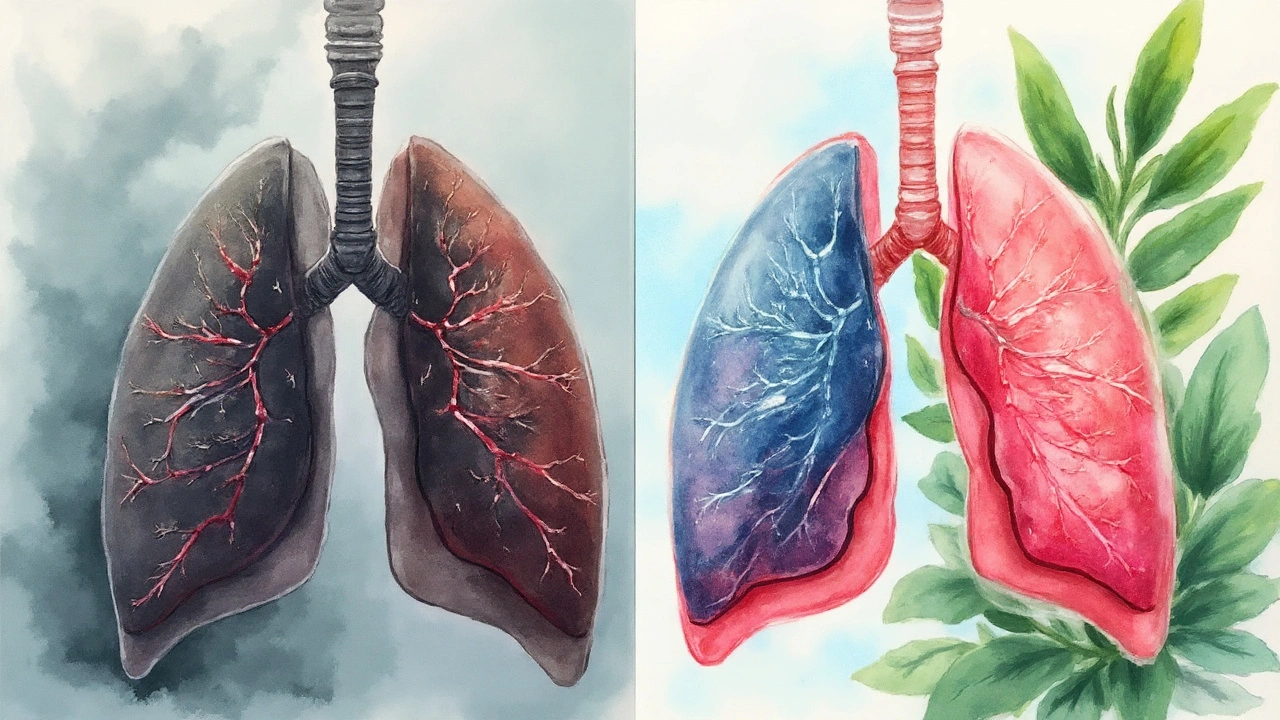
What Smoking Does on Its Own
Cigarette smoking is a tobacco‑combustion activity that delivers nicotine, tar, and over 7,000 chemicals into the lungs. The World Health Organization estimates 1.3billion people smoke worldwide, and each cigarette adds roughly 22minutes of life lost. The primary health impacts include:
- Respiratory disease: chronic obstructive pulmonary disease (COPD) affects 15% of long‑term smokers.
- Cardiovascular disease: smoking raises blood pressure, damages arterial walls, and triples the risk of myocardial infarction.
- Cancer: lung cancer accounts for 85% of all smoking‑related cancers, with a 20‑fold increase in odds.
What Alcohol Does on Its Own
Alcohol consumption refers to the intake of ethanol‑based drinks such as beer, wine, or spirits. Global per‑capita consumption averages 6.4liters of pure alcohol per year, and the WHO links alcohol to 3million deaths annually. Key health outcomes include:
- Liver disease: chronic heavy drinking leads to fatty liver, hepatitis, and cirrhosis, responsible for 1.5million deaths each year.
- Brain effects: alcohol alters GABA and glutamate transmission, impairing judgment and memory.
- Cancer: risk of oral, throat, breast, and liver cancers rises in a dose‑dependent way.
The Toxic Synergy: Why the Combo Is Worse
When cancer risk is evaluated for co‑consumers, epidemiological studies from the U.S., Europe, and Asia consistently show a multiplicative effect. For example, a 2023 meta‑analysis of 35 cohort studies found that smokers who drink ≥2 drinks per day have a 5‑fold higher odds of head‑and‑neck cancer than non‑smokers who abstain.
Two biological mechanisms drive this synergy:
- Carcinogen activation: alcohol induces the enzyme CYP2E1, which converts tobacco nitrosamines into more potent DNA‑damaging agents.
- Immune suppression: both nicotine and ethanol weaken immune surveillance, letting mutated cells proliferate unchecked.
Beyond cancer, the combination accelerates cardiovascular disease. A Finnish cohort of 12,000 adults showed that dual users had a 2.5‑times higher incidence of stroke than those who only smoked or only drank.
Why People Pair the Two
Social and neurochemical factors make the pairing almost inevitable in many cultures:
- Social context: Bars, nightclubs, and backyard gatherings often serve both cigarettes and drinks, reinforcing the habit loop.
- Neurotransmitter overlap: Nicotine spikes dopamine in the mesolimbic pathway, the same reward system activated by alcohol. The brain learns that the two together produce a stronger pleasure signal, deepening addiction.
- Stress relief myth: Both are perceived as anxiolytics, leading stressed individuals to reach for a cigarette while sipping a drink.
Public‑Health Policy: Targeting One Won’t Cut It
Many governments have rolled out successful anti‑smoking campaigns-plain packaging, high taxes, and smoke‑free laws-but they often treat alcohol policy as a separate beast. The result is a policy gap where dual users slip through the cracks.
Key policy recommendations include:
- Integrate warning labels: Include combined risk statements on cigarette packs and alcohol bottles.
- Co‑taxation: Align excise taxes for tobacco and alcoholic beverages to discourage simultaneous purchase.
- Venue restrictions: Ban smoking in bars and pubs, a strategy that already reduced secondhand smoke exposure by 70% in New Zealand.
- Funding for harm reduction strategies: Provide nicotine‑replacement therapy (NRT) alongside brief alcohol‑screening tools in primary‑care settings.
Dual‑Treatment Programs: The Most Effective Way Out
Research from the National Institute on Alcohol Abuse and Alcoholism shows that treating nicotine dependence in isolation yields a 20% relapse rate for alcohol, and vice‑versa. Dual‑treatment models-combining NRT, counseling, and medication‑assisted therapy for alcohol (e.g., naltrexone)-increase long‑term abstinence to over 45%.
Core components of a successful program:
- Screening: Simultaneously assess nicotine and alcohol use during every health visit.
- Motivational interviewing: Tailor messages that address the intertwined cravings.
- Pharmacotherapy: Pair varenicline (for nicotine) with acamprosate (for alcohol) when medically appropriate.
- Peer support: Offer group sessions where participants share strategies for handling social triggers like parties.
Practical Steps for Individuals
If you recognize the pattern in your own life, try these evidence‑based actions:
- Track triggers: Keep a diary of when you light up and what you were drinking. Notice if certain drinks (e.g., whiskey) make you reach for a cigarette.
- Separate the rituals: Replace the cigarette‑while‑drinking habit with a non‑nicotine alternative-chewing gum, a sip of water, or a quick walk.
- Set staggered goals: Quit smoking first, then reduce alcohol, or vice‑versa, based on which feels more manageable.
- Seek professional help: Ask your GP for a referral to a dual‑treatment clinic; many are now covered by public health insurance.
Related Concepts and Next Topics to Explore
The discussion of smoking‑and‑alcohol co‑consumption touches on broader subjects such as secondhand smoke exposure, alcohol‑related traffic accidents, and mental‑health comorbidities. Readers interested in digging deeper might look into:
- Smoking cessation methods: nicotine patches, e‑cigarettes, behavioral therapy.
- Alcohol moderation guidelines: standard drink definitions, low‑risk drinking limits.
- Public‑policy case studies: how New Zealand’s smoke‑free legislation reduced youth co‑use rates by 25%.
| Risk Category | Smoking Only | Alcohol Only | Smoking+Alcohol |
|---|---|---|---|
| Annual deaths (global) | 8million | 3million | ≈12million (synergistic) |
| Relative cancer risk (lung, throat, breast) | 2‑4× | 1‑2× | 5‑10× |
| Cardiovascular events | 3‑fold increase | 1.5‑fold increase | 4‑6‑fold increase |
| Average years of life lost | 10‑12years | 5‑7years | 15‑20years |
Take Action Today
The data are clear: smoking and alcohol together amplify danger, lock you into a stronger addiction loop, and strain public‑health resources. By recognizing the pattern, seeking dual‑treatment, and supporting policies that address both habits, you can break the cycle and reclaim healthier years.

Frequently Asked Questions
Does occasional smoking while drinking increase cancer risk?
Even occasional co‑use raises risk because alcohol enhances the activation of tobacco carcinogens. Studies show a 30‑40% rise in oral‑cavity cancer risk for people who smoke only on drinking nights.
Can I quit drinking first and then quit smoking?
Yes. The optimal order varies by individual. If alcohol is the stronger trigger for your smoking, tackling drinking first may reduce cravings for cigarettes. Consult a health professional for a personalized plan.
Are e‑cigarettes safer for people who also drink?
E‑cigarettes eliminate many combustion toxins, but nicotine still fuels the same dopamine pathway. They can help reduce smoking‑related lung damage, yet they do not mitigate the alcohol‑related risks. Dual‑treatment remains the gold standard.
What policy changes could curb co‑use?
Combined warning labels, synchronized taxation, and smoke‑free bar laws are top strategies. Funding for integrated screening in primary care also shows promise.
How does nicotine affect liver health when I drink?
Nicotine itself isn’t a liver toxin, but it can worsen alcohol‑induced inflammation by increasing oxidative stress. This dual assault speeds up the progression to fibrosis and cirrhosis.

Been trying to quit both for a year now. Switched to nicotine gum and sparkling water with lime-no more whiskey and smokes after work. Small wins, but it’s working. Thanks for the practical tips, this post actually helped me see the pattern.