When you walk into a hospital or clinic and wait for hours just to see a doctor, it’s not just bad luck. It’s the result of a system breaking under the weight of its own shortages. Hospitals and clinics across the U.S. are running on fumes-fewer nurses, fewer doctors, fewer support staff-and the people paying the price aren’t the administrators or the policymakers. They’re the patients.
What’s Really Going On Behind the Scenes?
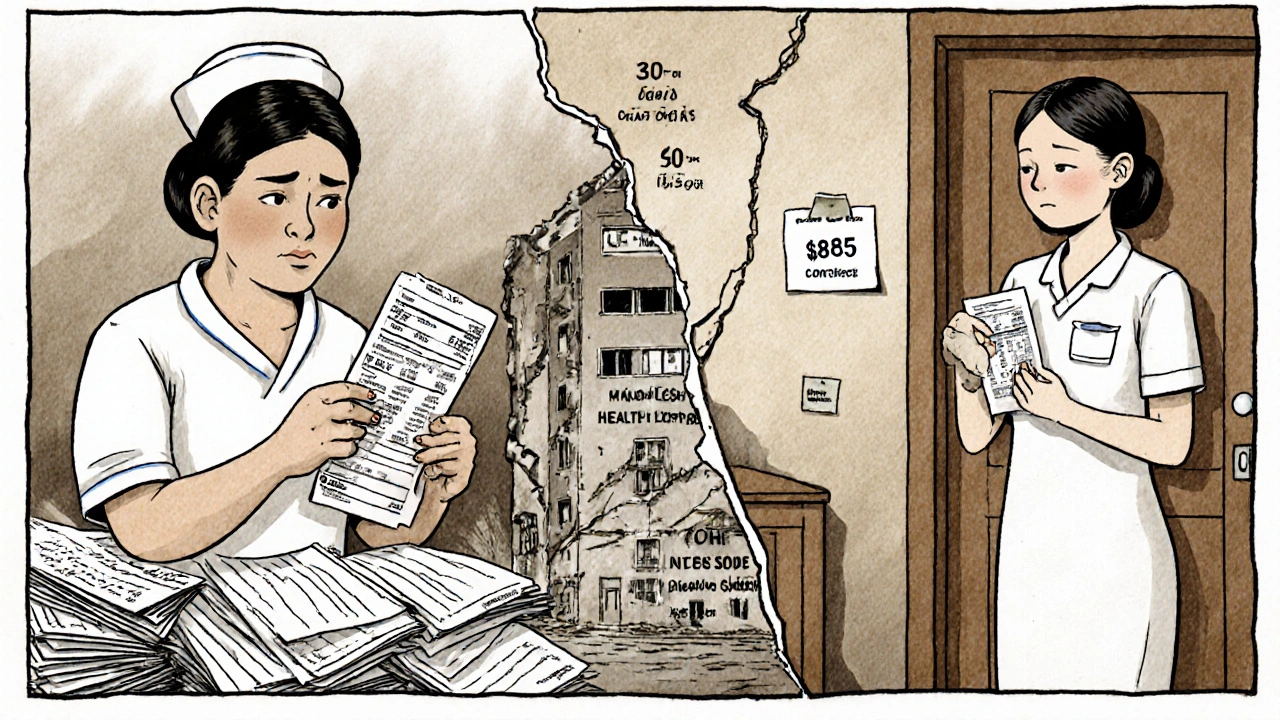
It’s not just one problem. It’s a chain reaction. The nursing shortage alone is projected to hit over 63,000 full-time equivalents by 2030. That’s not a number on a spreadsheet. That’s 63,000 shifts where someone has to cover for a colleague who quit, retired, or burned out. And it’s not just nurses. Primary care doctors are vanishing, especially in rural areas. Behavioral health providers? Nearly half the positions are empty. In 2024, rural clinics were operating at just 58% staffing levels. Urban clinics? Barely better at 79%. Meanwhile, hospitals in places like California are short by 45,000 nurses. In Nevada, patients are waiting up to 72 hours in emergency rooms just to be seen.
Why? Because the people who keep this system running are exhausted. Nearly half of all nurses are over 50. One-third will retire in the next 10 to 15 years. And the ones still working? Many are working 16-hour shifts with three patients each-double what’s considered safe. A 2022 study in JAMA found that when nurse-to-patient ratios go above 1:4, mortality rates jump 7%. That’s not a risk. That’s a death sentence waiting to happen.
Why Are People Leaving?
It’s not that nurses don’t care. It’s that they can’t take it anymore.
Turnover in nursing hit 104.4% in some specialties during the pandemic. That means, on average, every nurse in those units left and was replaced more than once in a single year. The reasons? Unsafe patient loads, mandatory overtime, emotional burnout, and pay that doesn’t match the toll. A travel nurse in New York might make $185 an hour, while a permanent staff nurse on the same floor makes $65. It’s no surprise people are walking out the door.
On Reddit, ICU nurse Sarah Chen wrote about working 16-hour days with three patients and nearly making two medication errors last month. On LinkedIn, hospital CEOs are admitting they’ve had to close 12 inpatient beds every week just because they don’t have enough staff. That’s not a temporary fix. That’s a system in collapse.
And it’s not just hospitals. Long-term care facilities are even worse off. They’re operating with 28% fewer nurses than before the pandemic. Elderly patients are getting less help bathing, eating, and turning in bed. Infections spread faster. Falls go unnoticed. People die because no one’s there to help.
What Happens When You Can’t Find a Doctor?
If you need a routine checkup, a mental health appointment, or even a simple prescription refill, you might be waiting weeks. In some areas, there’s not a single psychiatrist available for miles. Primary care clinics are turning away new patients because they’re already at capacity. And when people can’t get care early, their conditions get worse. Diabetes turns into amputations. High blood pressure turns into strokes. Depression turns into suicide.
Emergency rooms are the canary in the coal mine. The American College of Emergency Physicians reports that understaffed ERs now have 22% longer wait times than they did in 2022. That means someone having a heart attack might wait three hours before they even see a nurse. That’s not just inconvenient. That’s lethal.
Why Don’t We Just Hire More People?
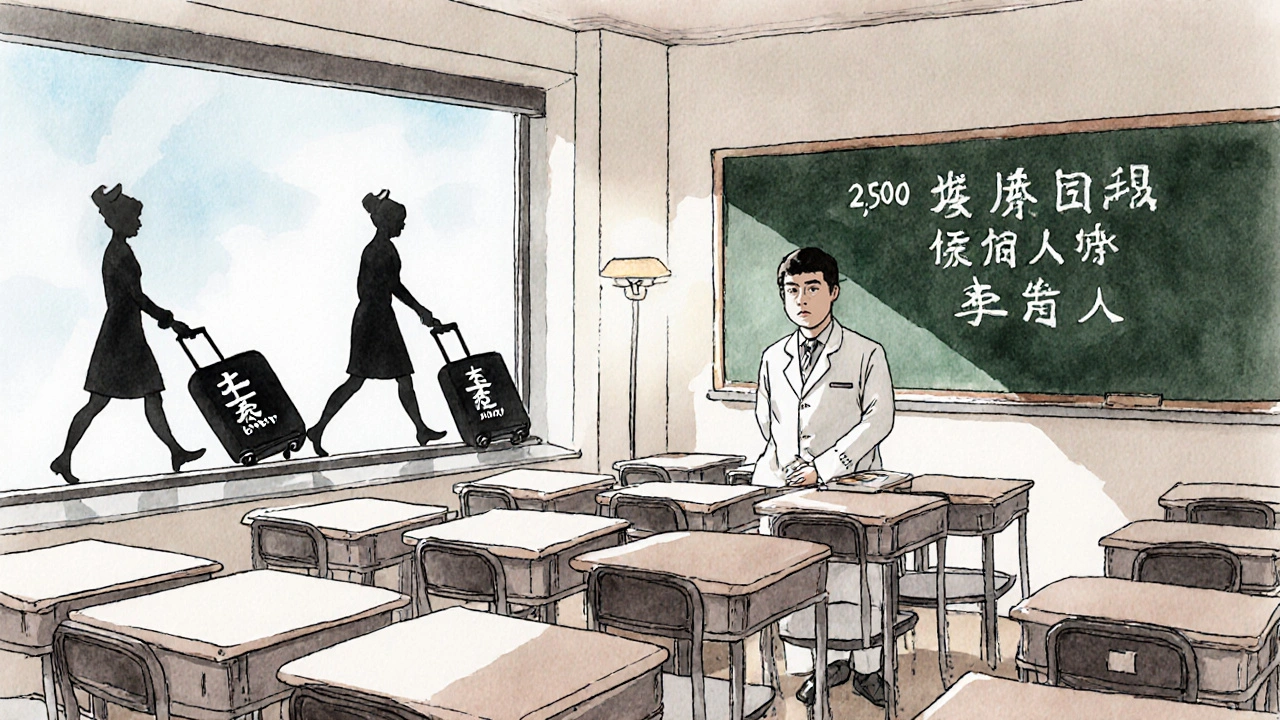
It sounds simple. But training a nurse takes years. Nursing schools are turning away over 2,300 qualified applicants every year-not because they don’t have space, but because they don’t have faculty. Eight percent of nursing professor positions are empty nationwide. No teachers. No new nurses.
And even when you do train someone, they don’t always stay. The average nurse leaves the profession within five years. Why? Because the system doesn’t support them. Hospitals spend millions on fancy technology but barely invest in mental health support for staff. Magnet hospitals-those with the best working conditions-give nurses 4.2 hours of professional development per month. Non-Magnet hospitals? Just 1.1 hours. It’s no wonder morale is low.
Some hospitals try to fix it with travel nurses. But that’s like patching a leaking roof with duct tape. Travel nurses filled 12% of hospital roles in 2023-but they cost 34% more. That money comes out of patient care budgets. Or worse, it means hospitals cut other services to pay for it.
Technology Isn’t the Magic Fix
Everyone talks about AI, telehealth, and automation as the solution. And yes, they help. Telehealth nurse triage reduced ER visits by 19% in pilot programs. AI tools can take over charting, freeing up nurses to focus on patients.
But here’s the catch: these tools need people to run them. You need nurses trained to use them. You need IT staff to keep them working. You need time to learn them. The learning curve for AI documentation tools? Over eight weeks. And 68% of hospitals can’t even get their electronic health records to talk to each other. That’s not innovation. That’s frustration.
Dr. Robert Wachter from UCSF says technology could offset 30-40% of staffing gaps. But he also says it won’t work unless we fix the culture first. You can’t slap an app on a broken system and expect it to heal.
What’s Being Done? And Is It Enough?
The Biden administration just allocated $500 million for nursing education and loan forgiveness. Sounds good, right? But the American Association of Colleges of Nursing says we need $1.2 billion just to meet demand. That $500 million covers 18% of what’s needed.
Some states are trying. California passed laws forcing hospitals to maintain safe nurse-to-patient ratios. Massachusetts uses loan forgiveness to keep nurses in the state. The results? Shortages there are 8% below the national average.
But most places? Nothing. Or worse-laws that make it harder. In 22 states, nurses can’t practice across state lines without going through a months-long licensing process. That’s 112 days on average. During a crisis, that’s a death sentence.
What This Means for You
If you’re healthy now, this might feel distant. But it won’t stay that way. By 2030, 42 states will have nursing shortages. By 2036, we’ll be short 86,000 doctors. The population over 65 is growing fast-55 million today, 82 million by 2050. And the number of working-age people to support each senior is dropping from four to less than three.
That means more people needing care. Fewer people to give it. And the system will keep getting worse until we treat this like the emergency it is.
It’s not about politics. It’s not about budgets. It’s about whether you or your parent or your child will get care when you need it most. Right now, the answer is: maybe not.
What Can Be Done?
There are no easy answers. But there are real ones.
- Invest in nursing education-fully, not half-heartedly. Pay professors. Fund scholarships. Let schools accept more students.
- Make nursing jobs sustainable. Cap patient ratios. Offer mental health support. Pay people fairly.
- Let nurses work across state lines. Remove licensing barriers that delay care by months.
- Use technology to support, not replace, people. Train staff. Fix broken systems first.
- Hold hospitals accountable. Tie Medicare payments to staffing transparency. No more hiding behind closed doors.
This isn’t about saving money. It’s about saving lives. And if we wait until the next crisis hits, it’ll be too late.
Why are hospitals closing beds due to staffing shortages?
Hospitals close beds because they don’t have enough nurses, doctors, or support staff to safely care for patients. Even if a bed is physically available, without staff to monitor patients, give medications, or respond to emergencies, it’s unsafe to use. Closing beds is a last resort to avoid putting patients and staff at risk.
Are travel nurses making the shortage worse?
Travel nurses fill critical gaps, but they’re not a long-term solution. They cost hospitals 34% more than permanent staff, which drains budgets. Their short-term contracts mean they move on quickly, leaving the same staffing holes behind. They help now, but they don’t fix the root problem: poor working conditions and low pay for permanent staff.
Why aren’t more people becoming nurses?
Many people want to become nurses, but nursing schools can’t accept them. There aren’t enough nursing professors-8.8% of faculty positions are empty. Even if someone gets in, the job itself is brutal: long hours, high stress, unsafe ratios, and low pay compared to the responsibility. That pushes many out before they even start.
How do staffing shortages affect patient safety?
When staff are stretched too thin, mistakes happen. Medication errors, missed vital signs, delayed responses to emergencies-all rise. Studies show a 7% increase in patient deaths when nurse-to-patient ratios exceed 1:4. In rural areas, patients wait days for care. That’s not negligence. It’s the system failing.
Is telehealth helping with the shortage?
Yes, but only in small ways. Telehealth nurse triage reduced ER visits by 19% in pilot programs. Remote monitoring helps manage chronic conditions. But it doesn’t replace in-person care for emergencies, surgeries, or complex cases. Plus, it requires staff trained to use it-and many hospitals still can’t get their systems to work together.
What’s the biggest barrier to fixing this crisis?
The biggest barrier is ignoring the human cost. Hospitals and governments keep looking for tech fixes or short-term staffing tricks. But until we pay nurses fairly, cap their workloads, support their mental health, and let them work without red tape, the crisis will only get worse. People aren’t machines. You can’t run a healthcare system on burnout.

So... we’re just letting people die because we’re too cheap to pay nurses enough to stay alive? I mean, come on. This isn’t rocket science.