Antibiotics are one of the most important medical breakthroughs in history. Before they existed, even a small cut or a sore throat could turn deadly. Today, they save millions of lives every year - but they’re not harmless. Using them without understanding how they work or what they can do to your body can lead to serious problems. This isn’t just about taking a pill when you feel sick. It’s about knowing which antibiotics are actually needed, what side effects to watch for, and why some of the most common ones might be doing more harm than good.
What Antibiotics Actually Do
Antibiotics don’t treat viruses. That’s a big mistake a lot of people make. If you have the flu, a cold, or most sore throats, antibiotics won’t help. They only work against bacteria. There are two main ways they fight infection: some kill bacteria outright (bactericidal), while others stop them from multiplying (bacteriostatic). This sounds simple, but it’s not always clear-cut in real life. A drug that kills bacteria in a lab might just slow them down in your body, and vice versa.
The first antibiotic, penicillin, was found by accident in 1928 when Alexander Fleming noticed mold killing bacteria on a Petri dish. That moment changed medicine forever. Since then, we’ve developed dozens of types - but not all are created equal. Today, the World Health Organization divides them into three groups to guide use: ACCESS (safe, first-choice), WATCH (higher risk of resistance), and RESERVE (only for last-resort cases). Misusing antibiotics pushes us toward a future where common infections become untreatable. Right now, drug-resistant infections kill over 1.2 million people each year globally.
The Top 7 Antibiotic Classes You’ll Actually Encounter
Most prescriptions fall into just a few categories. Here’s what you’re likely to be given, and what you need to know about each.
Penicillins
These are the oldest and still the most common. Amoxicillin alone accounts for nearly 18% of all antibiotic prescriptions in the U.S. - that’s over 120 million doses a year. It’s used for ear infections, sinus infections, strep throat, and pneumonia. The way it works is simple: it breaks down the outer shell of bacteria, making them burst.
Side effects? Nausea, stomach pain, and diarrhea are common. About 1 in 5 people get diarrhea. Yeast infections (especially in women) happen in 2-8% of users. But the biggest myth? Penicillin allergy. Around 10% of Americans say they’re allergic. Yet studies show 90% of those people aren’t actually allergic. They had a rash as a kid, or got sick while taking it, or were told they were allergic without testing. Getting tested can open up safer, cheaper options.
Cephalosporins
Cephalexin is the most used in this group, making up nearly 5% of all antibiotic prescriptions. It’s often given to people who think they’re allergic to penicillin - but the cross-reactivity is low. Only 1-3% of penicillin-allergic people react to cephalosporins.
They’re used for skin infections, urinary tract infections, and even some types of pneumonia. Side effects are similar to penicillins: diarrhea, nausea, and occasional rashes. Severe reactions like Stevens-Johnson syndrome are rare - fewer than 1 in 10,000 cases.
Tetracyclines
Doxycycline is the star here. It’s prescribed about 35 million times a year in the U.S. for acne, Lyme disease, and some respiratory infections. It works by blocking bacteria from making proteins they need to survive.
But it has serious rules. Don’t take it with dairy or antacids - they stop it from working. And never give it to children under 8. It permanently stains developing teeth. Adults get sunburns more easily while on it - photosensitivity affects 10-20% of users. A simple sunburn can turn into a blistering reaction. Always use sunscreen.
Macrolides
Azithromycin (brand name Zithromax) is the third most prescribed antibiotic in the U.S. It’s popular because you only take it for 3-5 days. It’s used for pneumonia, bronchitis, chlamydia, and strep throat.
Side effects? Stomach upset is common - 10-20% of users get nausea or diarrhea. But there’s a hidden risk: heart rhythm problems. Studies show azithromycin increases the chance of dangerous heart arrhythmias by over 2 times. This isn’t a big deal for healthy young people, but if you have heart disease or take other drugs that affect your rhythm, this could be dangerous. Always tell your doctor about your heart history.
Fluoroquinolones
Ciprofloxacin and levofloxacin are powerful. They’re used for serious infections like kidney infections, pneumonia, and some types of abdominal infections. But the FDA put a black box warning on them in 2016 - the strongest possible alert.
Why? Because they can cause permanent damage. Tendon rupture (especially in the Achilles) happens in 0.1-0.4% of users. Peripheral neuropathy - nerve damage causing numbness or burning pain - affects 0.2-0.5%. And research shows a 2.7 times higher risk of aortic aneurysm - a tear in the main artery. These aren’t rare side effects. They’re serious enough that doctors now avoid these drugs unless there’s no other option.
Sulfonamides
Trimethoprim-sulfamethoxazole (Bactrim or Septra) is still used for urinary tract infections and to prevent pneumonia in people with weak immune systems. It blocks bacteria from making folic acid, which they need to grow.
But it’s a high-risk drug. About 3-5% of users develop severe skin reactions. Stevens-Johnson syndrome - where your skin blisters and peels - can happen. It’s rare (1-6 cases per million), but deadly. If you get a rash, fever, or blisters while taking this, stop it immediately and go to the ER.
Glycopeptides
Vancomycin is the last line of defense. It’s used for MRSA - a superbug resistant to almost everything else. It’s given in the hospital through an IV. You won’t get this as an outpatient unless you’re very sick.
Side effects? If you get the infusion too fast, you can get “red man syndrome” - a sudden red rash, itching, and low blood pressure. It’s not an allergy; it’s a reaction to speed. Nephrotoxicity (kidney damage) happens in 5-30% of long-term users. Hearing loss is rare, but possible with high doses.
What Side Effects Are Most Common?
When patients are asked what bothers them most about antibiotics, the answer is almost always the same: diarrhea.
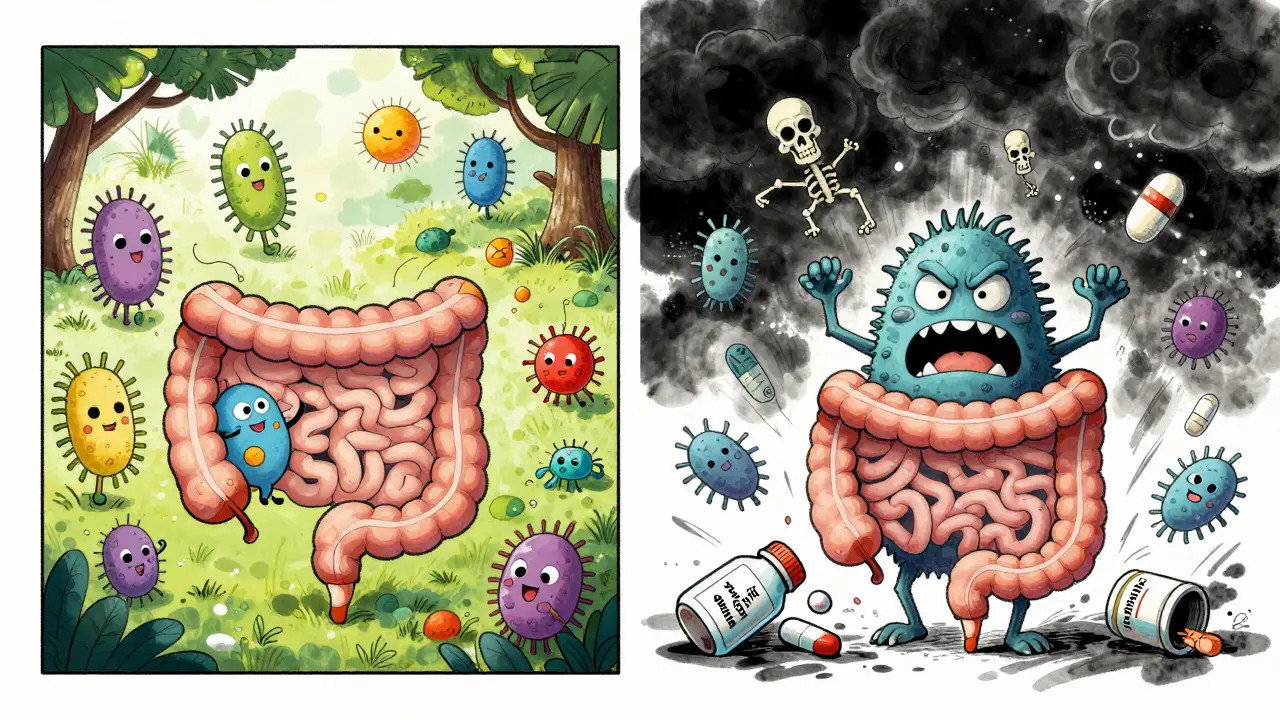
Studies from Drugs.com show 68% of users cite diarrhea as their top complaint. Why? Antibiotics wipe out good bacteria in your gut along with the bad ones. This lets yeast and other harmful bugs take over. Probiotics might help, but they’re not a magic fix. The best thing? Only take antibiotics when necessary, and finish the full course - even if you feel better.
Allergic reactions come second. About 22% of users report rashes, swelling, or trouble breathing. But again, many think they’re allergic when they’re not. A simple skin test can clear this up.
When Should You Say No?
Not every infection needs antibiotics. The CDC found that 45% of prescriptions for bronchitis - a viral illness - last longer than they should. Doctors often give them out of habit, or because patients demand them. But overuse is why we’re running out of effective drugs.
Ask your doctor: “Is this infection bacterial?” and “Is there a narrower-spectrum option?” If they say yes to both, you’re in good hands. If they say “it’s just easier to prescribe,” walk out. You’re not being difficult - you’re protecting yourself and the rest of us.

What’s Happening Now - And What’s Next
Only two new antibiotic classes have been approved since 2000. Why? Because they’re expensive to develop and don’t make much money. Companies don’t invest. Meanwhile, resistance keeps growing. MRSA resistance to vancomycin jumped from 0.3% in 2010 to 1.2% in 2022. That’s a fourfold increase.
But there’s hope. Hospitals in the U.S. now have mandatory antibiotic stewardship programs. These teams review every prescription to make sure it’s necessary. The result? A 35% drop in inappropriate use. And new drugs like cefiderocol are being tested for tough infections.
The bigger picture? The World Bank warns that by 2050, drug-resistant infections could cost the global economy $1 trillion a year. We’re not just talking about a few more deaths. We’re talking about a return to a time when a child’s scraped knee could kill them.
What You Can Do
- Don’t pressure your doctor for antibiotics. Ask if they’re needed.
- Never save leftover antibiotics for next time. They lose potency and can be dangerous.
- Finish the full course - even if you feel fine. Stopping early lets the toughest bacteria survive.
- Report side effects. Use the FDA’s reporting system. Your voice helps others.
- Get tested for penicillin allergy if you think you have it. You might be able to use safer drugs.
Can I take antibiotics if I’m allergic to penicillin?
Most people who think they’re allergic to penicillin aren’t. A skin test or graded challenge can confirm this. If you truly are allergic, there are other classes like cephalosporins (with only 1-3% cross-reactivity), macrolides, or sulfonamides. Always get tested before assuming you can’t take penicillin-based drugs.
Why do antibiotics cause diarrhea?
Antibiotics kill bacteria - including the good ones in your gut. This lets harmful bacteria like C. difficile overgrow, leading to diarrhea. In mild cases, it clears up after stopping the drug. In severe cases, it can cause life-threatening colitis. Probiotics may help, but the best prevention is only using antibiotics when absolutely necessary.
Are natural remedies like honey or garlic as good as antibiotics?
Honey and garlic have some antibacterial properties, but they’re not substitutes for prescription antibiotics. They might help with minor skin wounds or sore throats, but they won’t treat pneumonia, sepsis, or deep infections. Relying on them instead of antibiotics for serious infections can be deadly.
Can I drink alcohol while taking antibiotics?
For most antibiotics, alcohol is safe in moderation. But with metronidazole, tinidazole, or some cephalosporins, alcohol can cause severe reactions like vomiting, flushing, and fast heartbeat. Always check the label or ask your pharmacist. If you’re unsure, skip alcohol until you’re done.
Why are some antibiotics more expensive than others?
It’s not about effectiveness - it’s about patents and demand. Older antibiotics like amoxicillin cost pennies because they’re generic. Newer ones are expensive because they’re patented and harder to make. But cheaper doesn’t mean worse. In fact, doctors are encouraged to start with the cheapest, safest option first - unless there’s a clear reason not to.
What happens if I stop taking antibiotics early?
You might feel better, but the toughest bacteria survive. These are the ones that will come back stronger and harder to kill. This is how drug-resistant superbugs form. Even if you feel fine, finish the full course. It’s not about being “cured” - it’s about killing every last bacterium.
Let’s be real-antibiotics are the pharmaceutical equivalent of a sledgehammer to a hummingbird. We’re using Jenga blocks to fix a nuclear reactor, and somehow we’re surprised the whole thing’s about to implode. Penicillin? Sure, it’s the OG, but now we’ve got bacteria doing backflips around it. And don’t even get me started on fluoroquinolones-those things don’t just kill bacteria; they traumatize your tendons, your nerves, and your soul. The FDA’s black box warning? That’s not a warning-it’s a funeral notice for common sense.