When a doctor switches a patient from a brand-name drug to a generic version, most people assume it’s just a cost-saving move with no real difference. But for drugs with a narrow therapeutic index-often called NTI drugs-that assumption can be dangerous. These are the medications where even a small change in blood levels can mean the difference between treatment working and serious harm. Think blood thinners like warfarin, seizure drugs like phenytoin, or heart medications like digoxin. When generics are substituted without oversight, the risk isn’t theoretical. It’s real. And that’s where therapeutic drug monitoring (TDM) steps in-not as a luxury, but as a safety net.
What Makes a Drug an NTI? And Why It Matters
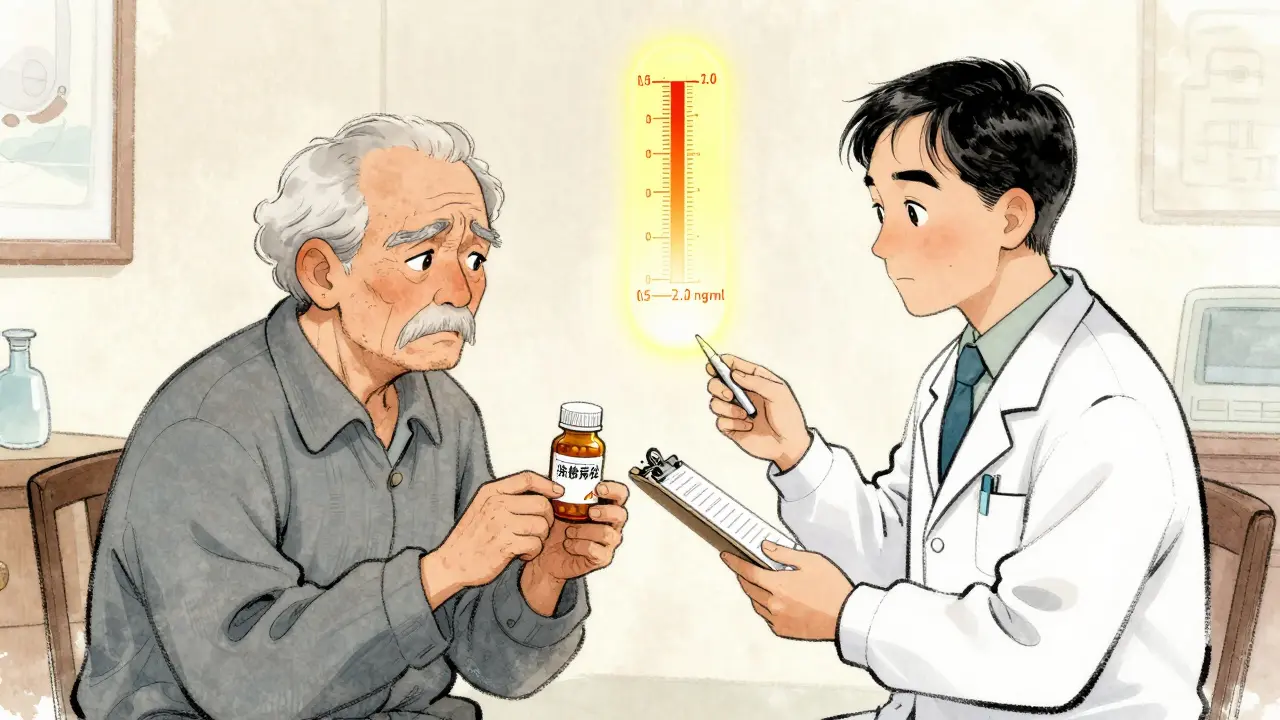
NTI stands for narrow therapeutic index. These drugs have a tiny window between the dose that works and the dose that causes harm. For example, digoxin, used for heart failure, has a therapeutic range of 0.5 to 2.0 ng/mL. Go below 0.5, and the heart condition worsens. Go above 2.0, and you risk fatal arrhythmias. That’s a 4-fold difference between safe and deadly.
Generics are required to be bioequivalent to the brand-name drug-meaning their absorption rate and total exposure should be within 80-125% of the original. Sounds close enough, right? But for NTI drugs, that 25% variation isn’t just a number. It’s a potential overdose or underdose. A 2018 study in the Journal of the American Pharmacists Association found that switching patients from brand to generic digoxin led to measurable changes in blood levels in 30% of cases. About 8% of those patients needed a dose adjustment within 30 days to avoid toxicity or treatment failure.
It’s not about quality. Generic manufacturers follow the same rules. But differences in inactive ingredients, tablet coating, or dissolution rates can alter how fast and how much of the drug gets into the bloodstream. For NTI drugs, those tiny differences add up fast.
Therapeutic Drug Monitoring: How It Works
Therapeutic drug monitoring isn’t a fancy lab test. It’s simple: measure the actual amount of drug in the patient’s blood, compare it to the known safe range, and adjust the dose if needed. It’s like checking your car’s oil level-not guessing, not assuming, just measuring.
For NTI drugs, TDM typically focuses on the trough level-the lowest concentration just before the next dose. This is when the drug’s effect is weakest, and if levels dip too low, the treatment fails. If they’re too high, toxicity kicks in.
The process looks like this:
- Doctor prescribes the generic version.
- After 5-7 days (when steady state is reached), a blood sample is drawn just before the next dose.
- The lab measures the drug concentration using a validated assay.
- The result is compared to the established therapeutic range.
- If outside range, dose is adjusted and rechecked in 1-2 weeks.
It’s not expensive. A single TDM test for digoxin or warfarin costs about $50-$80 in most U.S. labs. That’s less than one emergency room visit for a drug-related complication.
When TDM Is Most Critical
TDM isn’t needed for every patient on a generic NTI drug. But it’s essential in these cases:
- Patients switching from brand to generic, especially if they’ve been stable on the original.
- Older adults, whose metabolism slows and who often take multiple drugs.
- People with kidney or liver disease-these organs clear most NTI drugs.
- Patients on multiple medications that interact with the NTI drug (e.g., antibiotics changing warfarin levels).
- Pregnant women, where drug distribution changes dramatically.
A 2021 audit from the University of Wisconsin found that among 92 patients on generic phenytoin who had TDM done after a switch, 27% had levels outside the therapeutic range. Half of those were at risk of seizures or toxicity. All were corrected within two weeks of dose adjustment. No one was hospitalized.
The Cost of Not Monitoring
Some clinics skip TDM because they think it’s unnecessary. But the real cost isn’t the test-it’s the fallout.
In 2020, a CDC report linked 1,400 emergency room visits in the U.S. to NTI drug toxicity following generic switches. Most involved warfarin or phenytoin. One patient, a 78-year-old woman switched from brand to generic digoxin, developed ventricular tachycardia. Her level was 3.8 ng/mL-nearly double the safe limit. She spent 11 days in the hospital. Her total bill: $87,000. The TDM test? $65.
It’s not just about money. It’s about trust. Patients rely on their meds to work. When a switch causes a seizure, a bleed, or a heart rhythm problem, it shatters confidence in the system. TDM restores that trust by making sure the dose is right for the person, not just the pill.
Barriers to Widespread Use
So why isn’t TDM standard practice?
First, awareness. Many prescribers still believe generics are interchangeable without checking. Medical schools rarely teach NTI drug risks in depth.
Second, access. Not all labs offer TDM for NTI drugs. In rural areas, samples may need to be shipped, causing delays of 5-7 days. That’s too long if a patient is already symptomatic.
Third, reimbursement. Some insurance plans won’t cover TDM unless there’s a documented problem. But waiting for a crisis to justify testing defeats the purpose.
There’s also a myth that viral load or INR tests are enough. But INR only measures warfarin’s effect, not its concentration. And INR can be skewed by diet, alcohol, or other drugs. TDM gives the direct answer: how much drug is actually in the blood?
What Clinicians Can Do Today
You don’t need a fancy protocol to start protecting patients. Here’s what works:
- Know your NTIs. Warfarin, digoxin, phenytoin, carbamazepine, cyclosporine, theophylline, lithium. Keep a list handy.
- Test after every switch. Whether brand to generic or one generic to another, check levels 5-7 days later.
- Use local labs. Find a lab that offers rapid turnaround (under 48 hours). Some community hospitals can do it in-house.
- Document everything. Note the brand, generic name, dose, and date of switch. This helps track patterns.
- Don’t rely on patient reports alone. A patient might say they feel fine, but their digoxin level could be 3.2 ng/mL. That’s not fine.
A clinic in rural New Mexico started routine TDM after a patient died from phenytoin toxicity following a generic switch. They now test all patients on NTI generics. In two years, they’ve had zero hospitalizations related to these drugs.

The Bigger Picture
This isn’t just about generics. It’s about personalizing medicine. We don’t give everyone the same dose of insulin or thyroid hormone. Why do we assume the same dose of digoxin works for every person?
TDM for NTI drugs is one of the clearest examples of precision medicine that’s already here-low-tech, low-cost, and life-saving. It doesn’t require new drugs or complex tech. Just a blood draw, a lab, and the will to check.
As healthcare systems push for cost savings, we can’t afford to cut corners on safety. For NTI drugs, the cost of skipping TDM isn’t just financial. It’s measured in strokes, seizures, and lives lost.
Frequently Asked Questions
What drugs are considered NTI drugs?
NTI drugs include warfarin, digoxin, phenytoin, carbamazepine, cyclosporine, theophylline, and lithium. These have a very small range between effective and toxic doses. Even small changes in blood levels can lead to serious side effects or treatment failure.
Is TDM necessary for every generic drug?
No. Only for drugs with a narrow therapeutic index. For most medications like antibiotics or blood pressure pills, generics are reliably interchangeable. But for NTI drugs, even minor differences in absorption can be dangerous. TDM is not needed for drugs like metformin or atorvastatin.
How long does it take to get TDM results?
In most hospital labs, results take 24-48 hours. In rural areas or when samples are sent out, it can take 5-7 days. For urgent cases, some private labs offer 24-hour turnaround for an extra fee. Delayed results are the biggest barrier to timely adjustments.
Can TDM replace regular blood tests like INR for warfarin?
No. INR measures the effect of warfarin on clotting, not the actual drug level. TDM measures the concentration of warfarin in the blood. They’re complementary. INR is still needed for ongoing monitoring, but TDM helps explain why INR is off-especially after a generic switch or when drug interactions are suspected.
Is TDM covered by insurance?
Coverage varies. Many insurers cover TDM for NTI drugs if it’s ordered for a documented reason-like a recent generic switch, kidney disease, or suspected toxicity. Pre-authorization is often required. Some clinics bundle the test with routine labs to improve approval rates.
Next Steps for Patients and Providers
If you’re a patient on a generic NTI drug, ask your doctor: “Has my drug level been checked since I switched?” If you’re a provider, start with one NTI drug. Pick one patient after a switch. Order the test. Adjust if needed. Track the outcome. You’ll see the difference.
Protecting patients on generic NTI drugs isn’t about distrust in generics. It’s about respect for biology. Everyone metabolizes drugs differently. What works for one person might harm another. TDM doesn’t assume-it measures. And in medicine, that’s the most powerful tool we have.
so like... are you telling me the pharma giants are secretly making generics to fail on purpose? 😏 i mean, why else would they let people die from digoxin? someone's gotta be profit-ing off the ER visits. #BigPharmaIsWatching