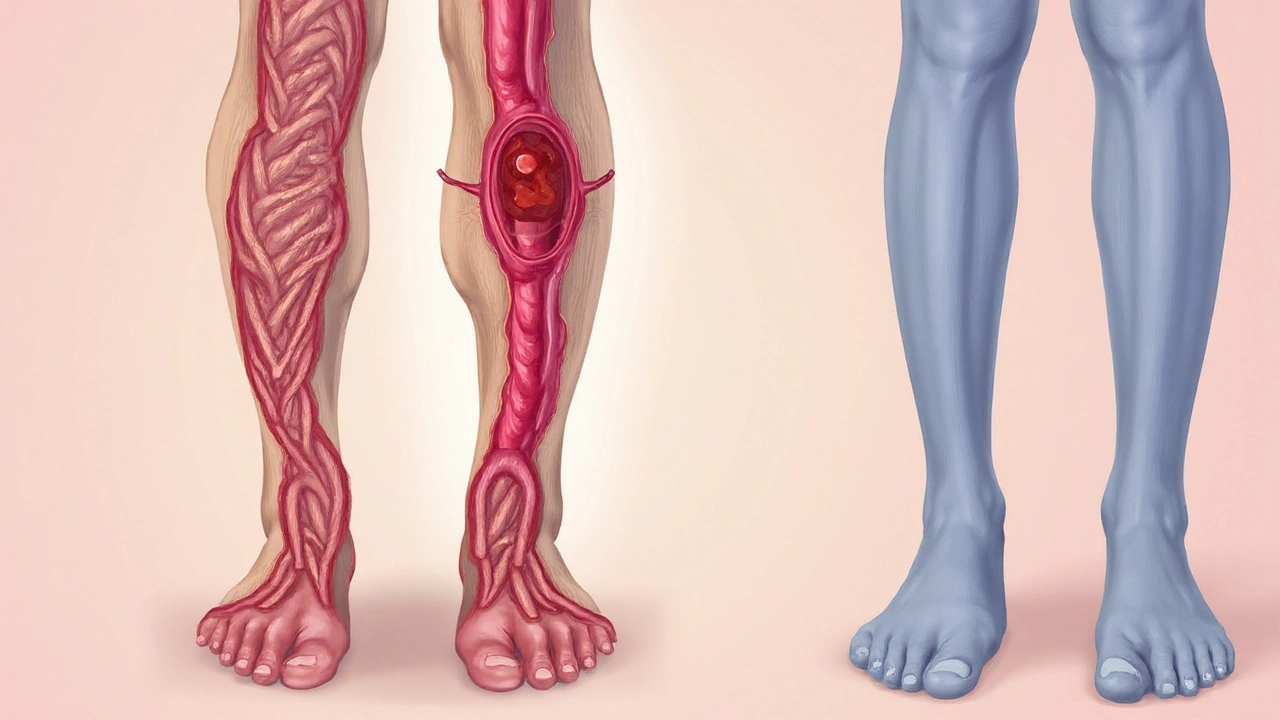
DVT is a blood clot that forms in a deep vein, most often in the legs, and can block blood flow back to the heart. When a clot travels to the lungs, it becomes a pulmonary embolism, a life‑threatening emergency. While DVT is a medical emergency, many people notice a quieter but persistent problem alongside it - varicose veins, swollen, twisted surface veins that usually appear on the calves or thighs, caused by weakened vein walls and faulty valves. Understanding how these two conditions intersect helps you spot warning signs early and act before complications arise.
What Exactly Is Deep Vein Thrombosis?
Deep vein thrombosis (DVT) occurs when a thrombus forms in the deep venous system. The clot often originates in the calf's venous sinus a channel that drains blood from the lower leg muscles and can extend upward. Classic symptoms include swelling, warmth, and a tight, painful feeling in the affected leg. However, up to 30% of DVT cases are silent, discovered only during imaging for another reason.
Varicose Veins: More Than a Cosmetic Issue
Varicose veins are visible, bulging vessels caused by chronic venous insufficiency the inability of vein valves to close properly, leading to blood pooling. While they often appear as blue‑purple cords, they can also bring aching, heaviness, and itching. If left untreated, they may ulcerate or become a breeding ground for clots.
Shared Risk Factors - The Overlap Zone
Both DVT and varicose veins share several triggers. The most significant is venous stasis a slowdown of blood flow in the lower extremities, which occurs during prolonged sitting, long‑haul flights, or pregnancy. Other common contributors include:
- Age over 60 - vein walls stiffen, and clotting factors increase.
- Obesity - excess weight compresses veins and raises inflammatory markers.
- Family history of clotting disorders such as thrombophilia genetic or acquired conditions that make blood extra prone to clotting.
- Hormonal influences - oral contraceptives or hormone replacement therapy boost clot risk.
- Inactivity - weak calf muscle pump fails to push blood upward.
When these factors are present, the same vein can develop a varicose appearance and simultaneously become a site for clot formation.
Pathophysiology: Why Varicose Veins Can Lead to DVT
The classic Virchow’s triad-stasis, endothelial injury, and hypercoagulability-explains clot formation. Varicose veins exacerbate two of these:
- Stasis: Dilated veins slow the return of blood, giving clotting factors more time to interact.
- Endothelial injury: The stretched vein wall becomes fragile, allowing tiny tears that expose tissue factor, a potent clot trigger.
In patients with an underlying hypercoagulable state elevated tendency for blood to clot, often due to genetic mutations like Factor V Leiden, the combination can rapidly progress from a simple varicose vein to a dangerous DVT.
How Doctors Diagnose the Connection
When a clinician suspects a link, they usually start with a physical exam: checking for palpable cords, skin changes, and asymmetrical swelling. The gold‑standard imaging tool is ultrasound Doppler a non‑invasive scan that visualizes blood flow and identifies clots in real time. The scan can simultaneously assess vein valve function, confirming chronic venous insufficiency.
Blood tests may include a D-dimer a fragment released when a clot breaks down, useful for ruling out DVT in low‑risk patients and a thrombophilia panel if a hereditary clotting disorder is suspected.
Management Strategies - Treating Both Issues Together
Because the conditions reinforce each other, a coordinated approach works best.
| Aspect | DVT | Varicose Veins |
|---|---|---|
| Primary cause | Blood clot in deep vein | Valve failure & vein dilation |
| Typical symptoms | Swelling, pain, warmth | Bulging veins, heaviness, itching |
| Risk of pulmonary embolism | High if untreated | Low, but clot can form in varicosities |
| First‑line treatment | Anticoagulant therapy | Compression stockings, lifestyle changes |
| Long‑term complications | Post‑thrombotic syndrome | Venous ulcers, chronic pain |
Anticoagulant therapy-usually a direct oral anticoagulant (DOAC) or low‑molecular‑weight heparin-prevents clot growth and new clots from forming. The treatment window typically lasts 3‑6 months, but patients with ongoing risk factors may stay on medication longer.
For varicose veins, compression stockings elastic garments that apply graduated pressure to aid venous return are the cornerstone. Class 2 (15‑20 mmHg) stockings are often prescribed for moderate disease, while higher grades are reserved for severe insufficiency.
In cases where clots form within a visibly varicose segment, doctors may consider a minimally invasive procedure called sclerotherapy injecting a solution that scars and closes the problematic vein. This not only removes the bulge but also reduces stasis, lowering future DVT risk.
Prevention - Keeping Your Legs Healthy
Adopting habits that improve blood flow lowers the odds of both conditions. Here are practical steps:
- Move every hour: Stand, stretch, or walk for at least two minutes during long trips or desk work.
- Exercise the calf pump: Heel‑raises, ankle circles, and swimming keep muscles contracting.
- Maintain a healthy weight: Even a 5% reduction can drop venous pressure noticeably.
- Stay hydrated: Thin blood flows more easily; aim for 2-3 liters of water daily.
- Wear appropriate footwear: Shoes with a slight heel encourage calf muscle activation.
- Consider prophylactic compression: Travelers on flights longer than four hours benefit from graduated stockings or inflatable foot cuffs.
If you have a family history of clotting disorders, ask your doctor about a baseline thrombophilia screen-early detection can guide personalized prevention plans.
When to Seek Medical Help
Because DVT can masquerade as a simple muscle ache, err on the side of caution. Contact a healthcare professional if you notice any of the following:
- Sudden swelling or redness in one leg.
- Sharp, unexplained pain while at rest.
- Warmth over a vein that feels hard to the touch.
- Newly worsening varicose veins accompanied by skin discoloration.
- Shortness of breath, chest pain, or coughing up blood - signs of a possible pulmonary embolism.
Prompt ultrasound assessment can rule out a clot and set you on the right treatment path.
Related Conditions Worth Knowing
Understanding the DVT‑varicose vein link opens the door to a broader network of vascular health topics:
- Chronic venous disease (CVD): The umbrella term covering varicose veins, edema, and skin changes.
- Post‑thrombotic syndrome: Long‑term pain and swelling after a DVT, often exacerbated by underlying venous insufficiency.
- Pulmonary embolism (PE): A clot that travels to the lungs; the most severe DVT complication.
- Peripheral arterial disease (PAD): Though a different vascular system, PAD can coexist and complicate leg symptoms.
Exploring each of these areas can help you develop a holistic view of leg health and avoid future surprises.
Key Takeaways
Deep vein thrombosis and varicose veins share a common enemy: poor venous circulation. By recognizing shared risk factors, monitoring symptoms, and acting early-whether through compression, anticoagulation, or lifestyle tweaks-you can dramatically lower the odds of a clot turning into a life‑threatening emergency.

Frequently Asked Questions
Can varicose veins cause a blood clot?
Yes. Dilated, valve‑fail veins create areas of slow flow and endothelial injury, which can seed a clot, especially if you have other risk factors like thrombophilia or prolonged immobility.
Is it safe to wear compression stockings if I already have DVT?
Compression is generally safe after the acute phase of a DVT (usually after 1‑2 weeks of anticoagulation) and can actually help prevent post‑thrombotic syndrome. Always follow your doctor’s guidance on the compression grade.
What lifestyle changes reduce both DVT and varicose vein risk?
Regular movement, calf‑strengthening exercises, weight control, adequate hydration, and avoiding tight clothing that restricts leg blood flow are the most effective habits.
Should I get screened for thrombophilia if I have varicose veins?
Screening is recommended if you have a family history of early clotting events, recurrent DVT, or unexplained clots at a young age. Your physician can order a panel that checks for Factor V Leiden, prothrombin mutation, and antiphospholipid antibodies.
How long does anticoagulant therapy last after a DVT?
Standard treatment is 3‑6 months. If you continue to have risk factors-like active cancer, ongoing immobility, or an inherited clotting disorder-your doctor may extend therapy indefinitely.

Ugh, another article that makes you feel guilty for sitting down. Like I don’t already know I should move more. But sure, let’s pretend I’m the villain here because my legs look like twisted ropes.