Sexual Side Effects Medication Checker
Many Common Medications Can Hurt Your Sex Life - And Most People Don’t Know It
You take your pill every morning like clockwork. Your blood pressure is under control. Your depression feels manageable. But lately, you’ve lost interest in sex. Maybe it’s harder to get or keep an erection. Or orgasms feel distant, even when you’re turned on. You feel embarrassed to bring it up - so you stay silent.
Here’s the truth: you’re not broken. You’re not alone. And it’s probably not your fault.
Between 25% and 73% of people taking antidepressants like SSRIs experience sexual side effects. That’s more than half. For some blood pressure meds, the number is just as high. Yet doctors rarely mention this before prescribing. Patients are left guessing why their sex life changed - and many stop taking their meds because of it.
This isn’t about shame. It’s about awareness. Let’s break down which medications cause sexual problems, how bad they really are, and what you can actually do about it.
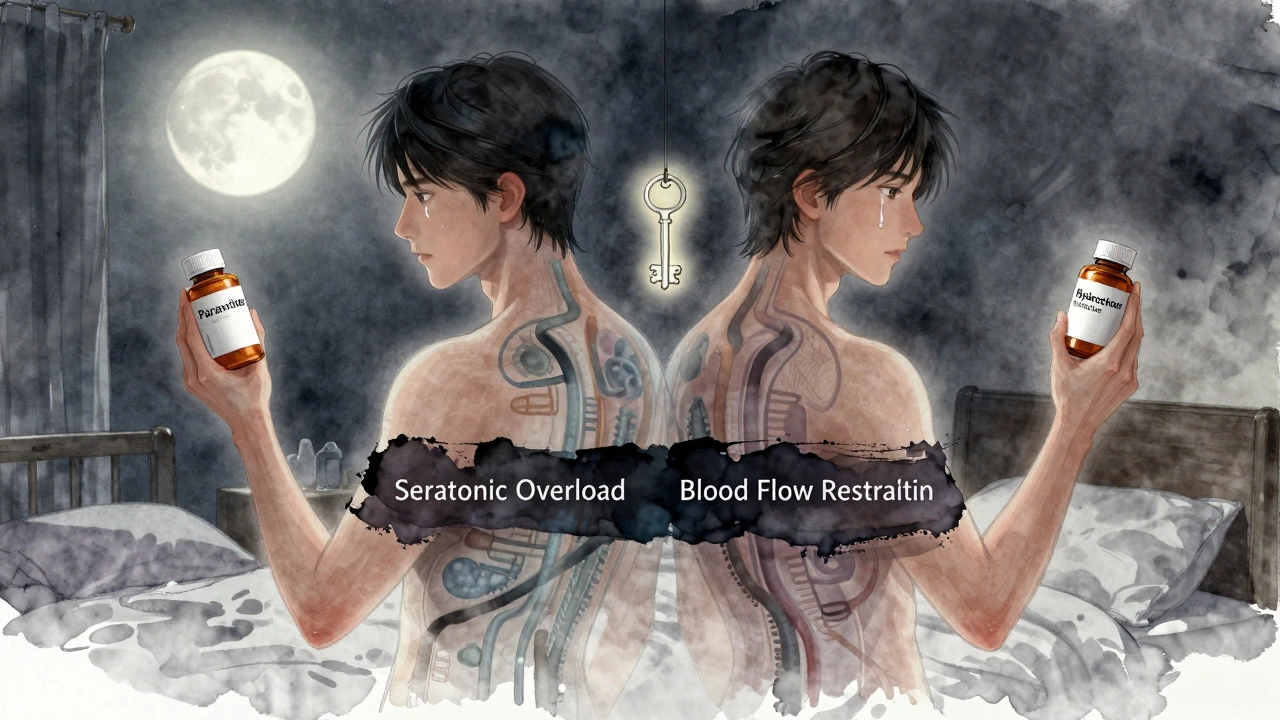
Antidepressants Are the Biggest Culprit - But Not All Are Equal
When it comes to sexual side effects, antidepressants lead the list. The most common offenders are SSRIs - selective serotonin reuptake inhibitors - like fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil).
Here’s what the numbers show:
- Paroxetine: 65% of users report sexual dysfunction
- Fluvoxamine: 59%
- Sertraline: 56%
- Fluoxetine: 54%
That’s not a typo. Nearly two out of three people on paroxetine struggle with low desire, delayed orgasm, or erectile problems. Even worse, one study found that 93% of people taking clomipramine (a tricyclic antidepressant) had trouble reaching orgasm at all - men and women alike.
But here’s the good news: not all antidepressants are created equal.
Bupropion (Wellbutrin) and mirtazapine (Remeron) have much lower rates of sexual side effects - often below 10%. Many doctors now start patients on these if sexual health is a concern. They work differently than SSRIs, and they don’t flood your system with serotonin the same way.
If you’re on an SSRI and your sex life has flatlined, switching isn’t a failure. It’s a smart adjustment.
High Blood Pressure Meds Are Quietly Sabotaging Your Libido
High blood pressure itself can lower sexual function. But the meds used to treat it? They make it worse.
Thiazide diuretics - like hydrochlorothiazide (Microzide) - are the most common cause of erectile dysfunction among heart medications. Up to 10% of heart failure patients say their sexual problems started after starting these pills.
Beta blockers like atenolol and metoprolol are next. They reduce blood flow and can make arousal harder, especially in women. Studies show 41% of women on these meds report lower desire, and 34% say sex feels less pleasurable.
But not all blood pressure drugs are bad for sex.
Valsartan and other angiotensin II receptor blockers (ARBs) have actually been linked to improved sexual desire and fantasies in women - compared to beta blockers. That’s not a fluke. It’s a clinically proven difference. If you’re on a beta blocker and your libido’s gone, ask your doctor if switching to an ARB is an option.
And don’t forget alpha-blockers like clonidine and prazosin. They’re used for high blood pressure and PTSD, but they also cut desire in half for some people. If you’re on one and feeling emotionally numb - not just depressed, but sexually numb - it’s worth discussing.
Prostate Meds and Antiandrogens: A Hard Trade-Off
Men taking medications for an enlarged prostate - like finasteride (Propecia, Proscar) or dutasteride - often face a tough reality. About 6-16% report lower libido. 5-9% get erectile dysfunction. And up to 21% have trouble with ejaculation.
Why? These drugs block DHT - a hormone that helps maintain prostate size but also supports sexual function. The trade-off? Fewer bathroom trips, but maybe fewer orgasms.
And then there’s prostate cancer treatment. Drugs like bicalutamide are antiandrogens - they shut down testosterone. The result? Nearly all men lose libido. Most get erectile dysfunction. Some develop breast tissue (gynecomastia).
These side effects aren’t rare. They’re expected. That’s why doctors now recommend talking about them before starting treatment. Knowing what’s coming helps men prepare mentally and emotionally. It doesn’t make it easier - but it makes it less isolating.
Other Surprising Offenders: Epilepsy Drugs, Opioids, and Acid Reflux Pills
It’s not just antidepressants and heart meds. A lot of everyday prescriptions can mess with your sex life.
Gabapentin and pregabalin (used for nerve pain and seizures) are linked to erectile dysfunction. They raise a protein that binds testosterone, leaving less of it free to do its job. That’s why some men on these meds feel like they’ve lost their drive - even if their mood is fine.
Opioids like oxycodone? They hit the brain’s hormone control center. Over time, they can cause secondary hypogonadism - meaning your body stops making enough testosterone. Result? Low sex drive, fatigue, and erectile problems. This isn’t just addiction-related. It happens even at prescribed doses.
And here’s one no one talks about: proton pump inhibitors (PPIs) like omeprazole (Prilosec) and H2 blockers like ranitidine. Some patients report lower libido and erectile issues. The science isn’t crystal clear yet, but the pattern is strong enough that doctors are starting to notice.
What You Can Do - Without Stopping Your Meds
You don’t have to suffer in silence. And you don’t have to quit your medication cold turkey. Here are realistic, doctor-approved options:
- Talk to your doctor - not your partner, not your friend, not Google. Your prescriber needs to know. They can’t help if they don’t know it’s a problem.
- Ask about switching - If you’re on paroxetine, could you try bupropion? If you’re on hydrochlorothiazide, could you try valsartan? These swaps are common and often effective.
- Try a "drug holiday" - For some SSRIs, taking a break on weekends (under medical supervision) can help restore sexual function without triggering withdrawal.
- Time your dose - Some people find taking their SSRI after sex - not before - reduces interference with arousal and orgasm.
- Add a PDE5 inhibitor - For men with SSRI-induced erectile dysfunction, sildenafil (Viagra) works in 74-95% of cases. It’s not a cure for low desire, but it can help with performance anxiety.
- Move your body - Exercise boosts blood flow, improves mood, and increases testosterone. Even 30 minutes of walking five days a week can make a difference.
Don’t wait until your relationship is strained or you’ve stopped taking your meds altogether. The earlier you speak up, the more options you have.
Why This Isn’t Just "In Your Head"
Some people say, "It’s all stress." Or, "You’re just anxious." But that’s not true.
Depression itself can lower libido - about 70% of people with depression have sexual issues even before taking meds. But when you add a drug that blocks serotonin pathways, it’s like pouring salt on a wound. The problem isn’t just your mental health. It’s the chemistry of the pill.
Same with high blood pressure. The disease causes vascular damage. The meds can make it worse. It’s not weakness. It’s biology.
And women? They’re often told their low desire is "normal" or "just aging." But when a woman on a beta blocker says she no longer feels turned on - even during intimate moments - that’s not normal. That’s a side effect.
These aren’t rare complaints. They’re predictable outcomes of well-studied drug actions. The real problem? Doctors aren’t trained to ask.
What’s Changing - And What to Watch For
Things are slowly getting better.
The FDA now requires drug makers to report sexual side effects in clinical trials for CNS medications. More studies are looking at how genetics affect your risk. Some new antidepressants are being designed specifically to avoid serotonin-related sexual problems.
The American Urological Association now recommends routine screening for sexual side effects in patients on long-term antidepressants, blood pressure meds, or prostate drugs. That’s progress.
But until your doctor asks you about your sex life - you have to bring it up.
Next time you’re in for a check-up, say this: "I’ve noticed my sex drive has dropped since I started [medication]. Is this a known side effect? Are there alternatives?"
That one sentence can change your quality of life.
Frequently Asked Questions
Can sexual side effects from medication be permanent?
For most people, sexual side effects go away after stopping the medication. But in rare cases - especially with long-term use of SSRIs or finasteride - some symptoms like low libido or erectile problems can persist. This is called Post-SSRI Sexual Dysfunction (PSSD) or Post-Finasteride Syndrome. It’s not common, but it’s real. If symptoms last more than a few months after quitting the drug, see a specialist.
Do all antidepressants cause sexual problems?
No. SSRIs like Prozac and Zoloft are the most likely to cause issues, but other classes like bupropion (Wellbutrin) and mirtazapine (Remeron) have much lower rates - often under 10%. If sexual health matters to you, ask your doctor about these alternatives before starting treatment.
Can I take Viagra with my antidepressant?
Yes, in many cases. Sildenafil (Viagra) and similar drugs like tadalafil (Cialis) are often prescribed alongside SSRIs to treat erectile dysfunction caused by the antidepressant. Studies show they work in 74-95% of these cases. But never combine them without your doctor’s approval - especially if you’re on nitrates or have heart conditions.
Why don’t doctors tell patients about this?
Many doctors assume patients won’t bring it up, or they think the mental health benefits outweigh sexual side effects. Some don’t know the full extent. Others fear causing anxiety. But research shows patients who are warned in advance cope better - even when side effects happen. It’s not about scaring people. It’s about informed consent.
Is it safe to stop my medication if I’m having side effects?
No. Stopping antidepressants or blood pressure meds suddenly can cause dangerous withdrawal symptoms, rebound hypertension, or worsening depression. Always talk to your doctor first. They can help you taper safely or switch to a better option.

I was on Zoloft for 3 years and my sex life went from "oh baby" to "oh whatever"... I thought I was broken until I read this. Then I switched to Wellbutrin and it's like I got my libido back. Also, I cry when I think about how many people suffer in silence. 😭