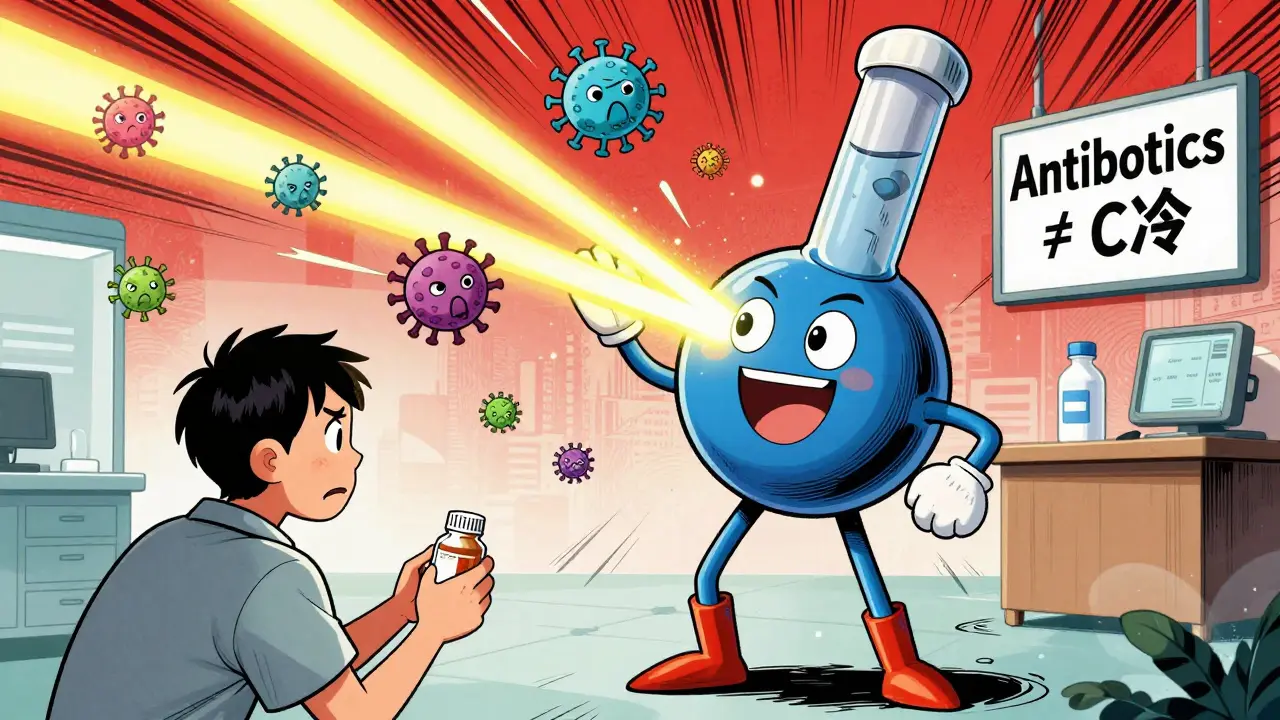
Antibiotics – What They Are and Why You Need Them
Antibiotics are medicines that kill or stop the growth of bacteria. They don’t work on viruses, so taking them for a cold or flu won’t help. Doctors prescribe them when a bacterial infection is confirmed or strongly suspected, because untreated infections can spread quickly and become serious.
Every pill, capsule, or injection contains a specific type of antibiotic designed to target certain bacteria. Knowing which one matches your infection is why a prescription matters.
How Antibiotics Fight Infections
Most antibiotics attack a bacterial process that human cells don’t need, such as building a cell wall or making proteins. When the drug blocks that process, the bacteria can’t multiply and eventually die off. Some antibiotics are “bactericidal” – they kill bacteria outright. Others are “bacteriostatic” – they just keep the bugs from growing, letting your immune system finish the job.
Common classes include penicillins, cephalosporins, macrolides, and fluoroquinolones. Each class has a typical spectrum: narrow‑range drugs hit only a few bacteria, while broad‑range ones hit many. Choosing the right spectrum helps avoid unnecessary damage to good bacteria in your gut.
Using Antibiotics Safely
The first rule is to finish the entire course, even if you feel better after a few days. Stopping early gives surviving bacteria a chance to adapt and become resistant.
Follow the dosage schedule exactly – take the medicine at the same times each day and with (or without) food as your doctor advises. Skipping doses creates low‑level exposure that encourages resistance.
Side effects are usually mild, like stomach upset or a rash. If you notice severe reactions – sudden fever, breathing trouble, or swelling – call a doctor right away. Probiotics can help keep your gut balance while you’re on a strong antibiotic.
Never share your prescription with anyone, and don’t use leftover pills for a new illness. Those leftover drugs may not match the new infection and can do more harm than good.
Resistance isn’t just an individual problem; it’s a public‑health issue. Overusing antibiotics in everyday colds, animal farming, or unnecessary prescriptions speeds up the rise of “superbugs” that no drug can defeat.
To protect yourself, ask your doctor if a test can confirm a bacterial cause before starting treatment. If a viral infection is likely, ask about supportive care instead of an antibiotic.
Our site offers more articles that help you stay healthy – from diet tips that support gut flora to safe ways to manage common infections without drugs. Browse the tag for practical health guides that fit a busy lifestyle.
Remember: antibiotics are powerful tools, but they work best when you use them exactly as prescribed, finish the whole pack, and keep good communication with your healthcare provider. By following these simple steps, you protect your health today and help keep these medicines effective for tomorrow.
Antibiotics: Most Common Types and Their Side Effects
Antibiotics save lives, but misuse and side effects are rising. Learn the most common types - from penicillin to vancomycin - and what they really do to your body. Know the risks, when to say no, and how to protect yourself.
More Detail
Antibiotics for Bacterial Infections: Classes and How They Work
Learn how different classes of antibiotics target bacterial infections, why they work-and why misuse leads to dangerous resistance. Essential facts for informed health decisions.
More Detail
Antibiotics for Bacterial Vaginosis: Benefits, Risks, and What to Expect
Explore how antibiotics treat bacterial vaginosis, their pros and cons, side‑effects, resistance issues, and alternative approaches to help you decide the best course.
More Detail