Every time you pick up your blood pressure or diabetes meds, you’re paying the same copay-whether you get 30 days or 90 days of pills. That’s not a mistake. It’s a hidden savings opportunity most people never ask for.
If you take the same medication every month, you’re probably paying for it three times a year. But what if you could get all three months at once… and pay the same price as one? That’s not a fantasy. It’s a standard option with most insurance plans in 2025. And it could save you up to $40 a year per medication-without changing anything else.
Why 90-Day Fills Save Money
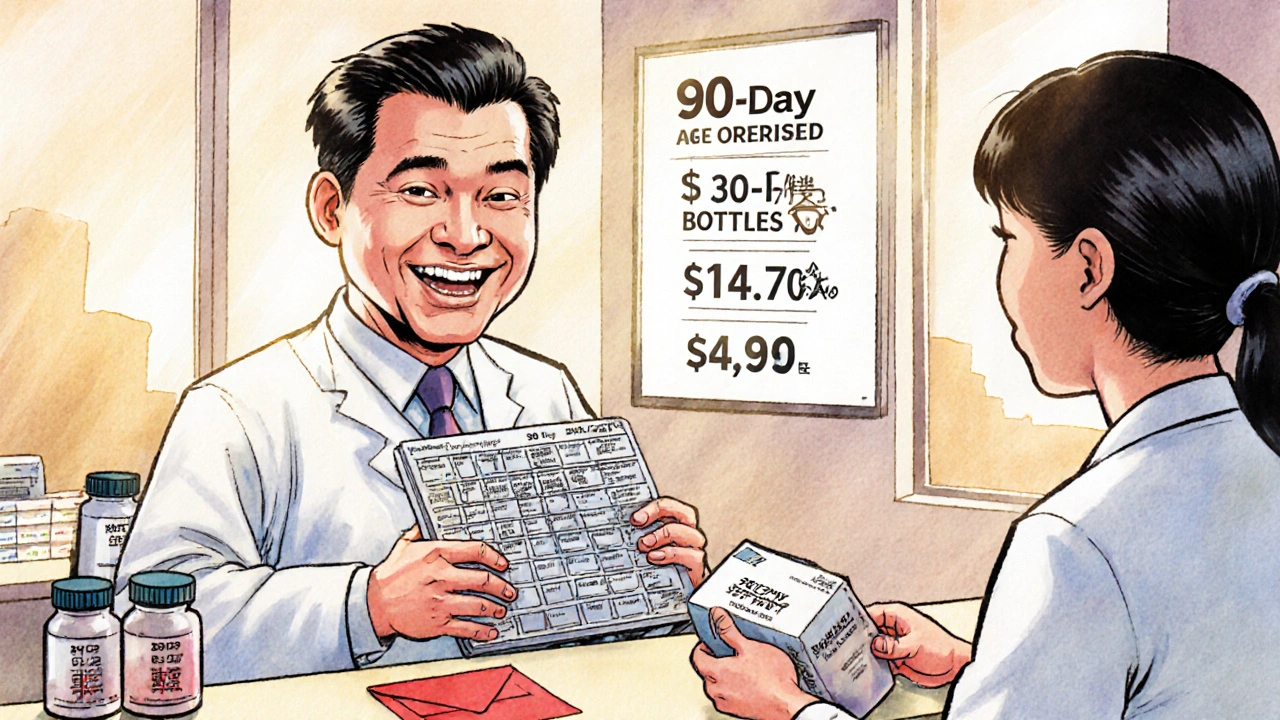
Here’s how it works: your insurance sets a flat copay for each prescription fill. Let’s say your copay is $4.90 for a 30-day supply. If you refill every month, you pay $14.70 every three months. But if you get a 90-day supply in one go, you still pay $4.90-no extra charge. That’s $9.80 saved every three months. Over a year, that’s almost $40 on just one drug.
This isn’t just about the math. You’re also saving time. Instead of making three trips to the pharmacy each year, you make one. No more running out on a weekend. No more forgetting to call in a refill. For people managing chronic conditions like high cholesterol, thyroid issues, or asthma, that consistency matters. Studies show people who get 90-day fills are far more likely to take their meds as prescribed.
Mail-order pharmacies like CVS Caremark or Postal Prescription Services (PPSRX) often offer 90-day fills with free shipping. But you don’t have to wait for pills to arrive. Many retail pharmacies now offer 90-day fills right at the counter. You walk in, ask for it, and walk out with three months’ worth-same as always.
Who Qualifies for a 90-Day Fill
Not every drug is eligible. Insurance companies only allow 90-day fills for maintenance medications-drugs you take daily for long-term conditions. That includes:
- Blood pressure meds (like lisinopril or amlodipine)
- Cholesterol drugs (like atorvastatin or rosuvastatin)
- Diabetes medications (like metformin or glimepiride)
- Thyroid pills (like levothyroxine)
- Antidepressants (like sertraline or escitalopram)
- Asthma inhalers (like fluticasone)
You also need to have taken the medication before. You can’t get a 90-day supply on your first prescription. Insurance wants to make sure you tolerate it well. If you just started the drug last month, you’ll need to wait until you’ve had at least one 30-day refill.
Some drugs are excluded-like antibiotics, painkillers, or short-term treatments. Those are meant to be used for a few days or weeks. But if you’ve been on a medication for three months or more, you’re likely eligible.
How to Get a 90-Day Prescription
Getting a 90-day fill is simple. You don’t need special paperwork or a new doctor’s visit. Here’s what to do:
- Check your prescription label. Look at the number of refills left. If you have at least two refills, you can ask your pharmacy to dispense a 90-day supply now. They can legally split a 30-day prescription into a 90-day supply if there are enough refills.
- Call your doctor. If you only have one refill left-or none-ask your doctor to write a new prescription for 90 days. Most doctors will do this without hesitation. It’s easier for them too. Fewer refill calls, fewer errors.
- Choose your pickup method. You can get it at your local pharmacy or use mail-order. Mail-order is often cheaper and comes with free shipping. Retail pharmacies are more convenient if you need it right away.
- Confirm your copay. Always ask: “What’s my copay for a 90-day supply?” Some plans offer even lower rates for longer fills. Don’t assume it’s the same as 30 days-ask.
Pro tip: Don’t wait until your last pill is gone. Start the process when you have 10-15 days left. That way, you won’t run out if there’s a delay.

Mail-Order vs. Retail Pharmacy
There are two main ways to get your 90-day supply: mail-order or in-store.
Mail-order pharmacies (like CVS Caremark, Express Scripts, or HPSM’s PPSRX) specialize in long-term meds. They send your pills in bulk, usually with free shipping. Many offer automatic refills-you don’t even have to call. You’ll typically pay the lowest possible copay, sometimes as low as $0 for generics. But you have to wait 7-10 days for delivery.
Retail pharmacies (CVS, Walgreens, Rite Aid, local independents) now offer 90-day fills right at the counter. You can pick it up the same day. It’s great if you need your meds fast or don’t trust mail delivery. Some retail pharmacies even match mail-order prices.
Compare both. If your plan lets you choose, check the price for each option. Sometimes the retail pharmacy is cheaper, especially if you’re using a discount app like GoodRx. But for most people, mail-order wins on price and convenience.
What to Watch Out For
It’s not always smooth sailing. Here are the common roadblocks-and how to fix them:
- “We don’t do 90-day fills here.” That’s usually not true. Ask to speak to the pharmacist. Retail pharmacies are required to honor your insurance’s 90-day benefit. If they refuse, call your insurer.
- “Your plan doesn’t cover it.” Check your plan’s formulary or call member services. Some plans only allow 90-day fills through mail-order. Others restrict certain drugs. Ask: “Is [medication name] eligible for a 90-day supply under my plan?”
- “I need prior authorization.” Some drugs require approval before the pharmacy can dispense a 90-day supply. Your doctor can submit this in minutes. Don’t give up-just ask your pharmacy to start the process.
- “I’m worried about waste.” If you stop the medication or switch to something else, you’ll have leftover pills. That’s fine. Most plans allow you to return unused pills for credit. Ask your pharmacy about their return policy.
If you’re on Medicare Part D, Medicaid, or a commercial plan from UnitedHealth, CVS, or Kaiser, 90-day fills are almost certainly covered. If you’re unsure, just call your insurer. They’ll tell you in under five minutes.
Real Savings, Real Impact
In 2025, about 12% of maintenance medications in the U.S. are filled as 90-day supplies. That’s already saving consumers and employers over $600 million a year. If adoption jumped to 70%, that number could hit $23 billion over ten years.
For you, that means real cash in your pocket. If you take three maintenance drugs, you could save $120 a year. That’s a weekend trip, a new pair of shoes, or a month of your gym membership.
And it’s not just about money. People who get 90-day fills are less likely to miss doses. That means fewer hospital visits, fewer complications, and better health long-term. It’s one of the simplest, most effective ways to take control of your health-and your budget.
Next Steps
Here’s what to do right now:
- Look at your medicine cabinet. Which pills do you take every day?
- Check the label on your most recent prescription. How many refills do you have left?
- Call your pharmacy and ask: “Can I get a 90-day supply of [medication name]?”
- If they say no, ask to speak to the pharmacist-or call your insurance provider directly.
- If you have two or more refills left, ask them to fill it now.
- If you’re out of refills, call your doctor and ask for a new 90-day prescription.
It takes less than 10 minutes. And the savings last the whole year.
Can I get a 90-day supply for any medication?
No. Only maintenance medications for chronic conditions qualify-like blood pressure, diabetes, cholesterol, thyroid, or asthma drugs. You can’t get 90-day fills for antibiotics, painkillers, or short-term treatments. Your insurance plan will specify which drugs are eligible.
Do I need a new prescription from my doctor?
Not always. If your current prescription has at least two refills left, your pharmacy can give you a 90-day supply without a new script. But if you’re out of refills, or your doctor wrote the prescription for only 30 days with no refills, you’ll need to call them for a new 90-day prescription. Most doctors are happy to do this.
Is mail-order safer than picking up at the pharmacy?
Yes. Mail-order pharmacies are licensed and regulated just like retail pharmacies. Pills are sealed, labeled, and shipped under strict conditions. Many offer tracking and temperature-controlled packaging for sensitive meds. If you’re concerned about delays, choose a plan with automatic refills and a backup supply.
What if I don’t like the medication after 90 days?
If you stop taking the drug or switch to something else, you can usually return unused pills to the pharmacy for a partial refund. Policies vary by plan, so ask ahead of time. Most insurers allow returns of unopened, sealed medication within 30 days of delivery.
Will my copay be the same for 90-day fills?
Usually, yes. Most plans charge the same copay for 90-day fills as they do for 30-day fills. Some even offer lower copays for the longer supply. Always confirm your cost before filling. If your copay is higher for 90 days, ask if you can switch to mail-order or another pharmacy.
Can I use GoodRx with a 90-day fill?
Yes. GoodRx can be used at retail pharmacies for 90-day fills. It’s especially helpful if your insurance doesn’t cover the drug well-or if you’re paying cash. Compare the GoodRx price with your insurance copay. Sometimes GoodRx beats your plan, even for 90-day supplies.
Why do some pharmacists seem reluctant to give 90-day fills?
Some retail pharmacies make less money on 90-day fills because they get paid per dispensing, not per pill. Fewer refills mean fewer fees. But that doesn’t mean they can refuse you. Your insurance plan requires them to honor your benefit. If a pharmacist pushes back, ask to speak to the manager or call your insurer directly.
This is how they get you hooked. One day you're saving $40, next thing you know, Big Pharma's got your whole life mapped out.