Bromocriptine Timing Calculator
How Timing Affects Your Medication
Bromocriptine must be taken within 2 hours of waking to effectively reset your body's circadian rhythm. Missing this window reduces effectiveness by up to 0.7% in HbA1c reduction. Consistency matters more than exact timing.
Your dose window will appear here with personalized advice based on your timing.
Why Bromocriptine Is Different From Other Diabetes Drugs
Most diabetes medications work by pushing insulin out of the pancreas, helping cells absorb sugar, or blocking sugar absorption in the gut. Bromocriptine - sold as Cycloset - does none of that. Instead, it talks to your brain. Specifically, it targets dopamine receptors in the hypothalamus, the part of your brain that controls your body’s daily rhythm. This isn’t just about blood sugar. It’s about resetting your internal clock to reduce the morning surge of stress hormones that make insulin less effective.
Approved by the FDA in 2009, bromocriptine isn’t a first-line drug. It’s not as strong as metformin at lowering HbA1c - it typically brings it down by 0.4% to 0.8%, compared to metformin’s 1.1%. But here’s what makes it stand out: in a 52-week study, patients taking bromocriptine had a 40% lower risk of heart attack, stroke, or heart-related death than those on placebo. That’s rare. Most diabetes drugs don’t do that. For people with existing heart disease who can’t take metformin, this drug can be a lifeline.
The Timing Rule That Makes or Breaks Bromocriptine
You can’t take bromocriptine at lunch. Or dinner. Or right before bed. It has to be taken within two hours of waking up. Not “when you feel like it.” Not “after coffee.” Within two hours of when you first open your eyes.
Why? Because your body’s sympathetic nervous system spikes in the early morning - releasing hormones that raise blood sugar. Bromocriptine works by calming that spike. If you take it too late, it misses the window. Clinical trials showed patients who took it within that two-hour window had 0.7% greater HbA1c reduction than those who didn’t. That’s the difference between a good result and no result.
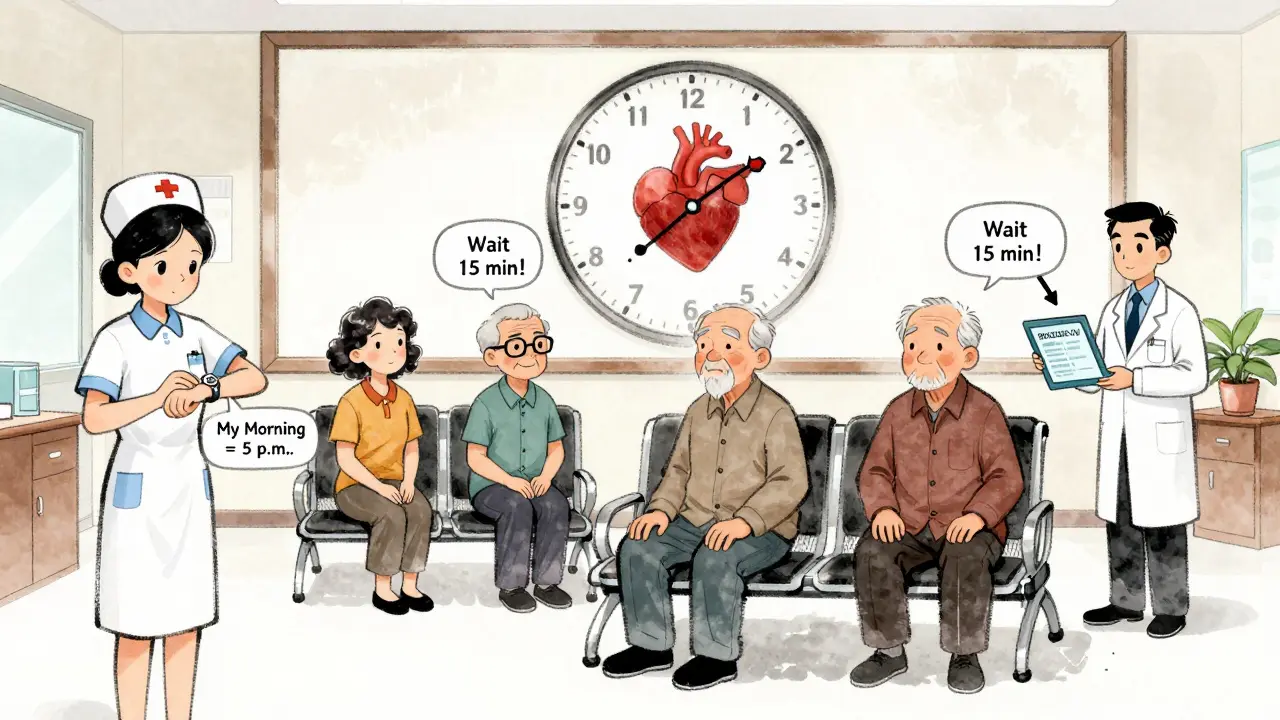
For night shift workers, people with irregular sleep, or those who sleep in on weekends, this is a major hurdle. One patient on Reddit said, “I’m a nurse who works nights. My ‘morning’ is 5 p.m. Do I take it at 5 p.m. or 7 a.m.? My doctor didn’t know.” That’s the problem. The drug only works if your body expects it at the same time every day - aligned with your natural wake cycle. If your wake time changes, you need to adjust the dose time accordingly. Consistency matters more than the exact hour.
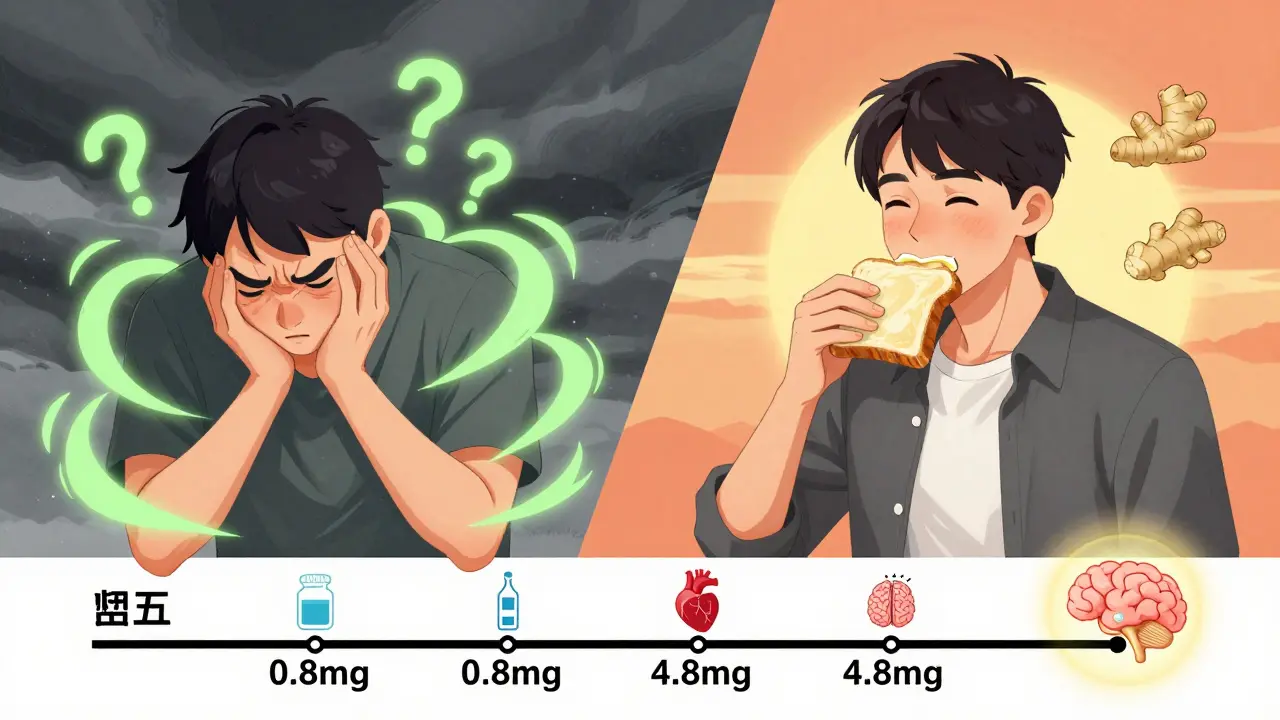
Nausea: The Most Common Reason People Quit
One in three people starting bromocriptine quits because of nausea. It’s not mild. It’s the kind that makes you feel like you’re going to throw up, especially in the first two weeks. Studies show 26% to 32% of users experience it. That’s way higher than metformin (5-10%) or DPP-4 inhibitors (under 10%).
But here’s the good news: it usually gets better. The key is how you start. Most doctors prescribe it at 0.8 mg daily and slowly increase by 0.8 mg each week until reaching 4.8 mg. If you jump straight to the full dose, nausea hits hard. If you go slow, it drops from 32% to just 18%. One patient wrote on Drugs.com: “I almost quit after day two. My doctor told me to start at 0.8 mg and take it with a piece of toast. By week three, I barely noticed it.”
What helps? Take it with a small amount of dry food - one or two crackers, half a slice of toast, or a few almonds. Don’t take it on an empty stomach. Avoid liquids for 30 minutes after. Some people swear by ginger: 250 mg of ginger supplement 30 minutes before the dose reduced nausea severity by 40% in one small study.
Dizziness: What to Expect and How to Handle It
Dizziness affects about 11% to 15% of users. It’s not the spinning kind. It’s more like a sudden lightheadedness right after standing up - like you’re about to pass out. It usually lasts 15 to 30 minutes and fades as your body adjusts.
Why does it happen? Bromocriptine can lower blood pressure slightly, especially when you stand up too fast. The risk is higher in older adults or people already on blood pressure meds. The fix? Don’t jump out of bed. Sit on the edge for a minute. Then stand slowly. Wait 15 to 20 minutes before doing anything that requires balance - like driving or showering.
Most people report the dizziness disappears after 2 to 4 weeks of consistent dosing. If it doesn’t, talk to your doctor. It could be a sign you’re on too high a dose or that another medication is interacting.
Who Should Consider Bromocriptine - And Who Should Avoid It
This drug isn’t for everyone. It’s best suited for people who:
- Have type 2 diabetes and established heart disease
- Can’t take metformin due to stomach issues or kidney problems
- Have a consistent morning routine
- Are willing to stick with the slow dose increase
It’s not a good fit if you:
- Work night shifts or have wildly irregular sleep
- Have a history of fainting, syncopal migraines, or low blood pressure
- Have severe kidney disease (eGFR under 30)
- Are looking for quick, strong blood sugar drops
It’s also not for people who want to lose weight - it’s weight-neutral. And it won’t cause low blood sugar on its own, which is a big plus compared to sulfonylureas or insulin.
Real-World Use: Why Fewer Doctors Prescribe It
Despite its unique benefits, bromocriptine makes up less than 1% of the diabetes drug market. Why? Two reasons: timing and side effects.
Most primary care doctors don’t have the time to explain the strict dosing window or manage the nausea. Endocrinologists prescribe it 68% of the time. That’s because they’re more familiar with the nuances - how to titrate slowly, how to handle dizziness, and how to reinforce the morning routine.
There’s also a lack of big, long-term studies. The main cardiovascular benefit data comes from one 52-week trial with just over 3,000 patients. While promising, some experts say we need larger trials before calling it a standard option. That’s why the American Diabetes Association calls it a “reasonable option for select patients” - not a first choice.
But here’s what’s changing: a new trial called BROADEN-CV, with 3,500 patients, is wrapping up in late 2025. If it confirms the heart benefits, bromocriptine could get a bigger role in guidelines.
How to Make It Work: A Simple Daily Plan
If you’re starting bromocriptine, here’s what to do:
- Set a daily alarm - not for waking up, but for taking the pill. Put it right next to your bed.
- Start low - 0.8 mg for 7 days, then 1.6 mg, then 2.4 mg, and so on, up to 4.8 mg over 6 weeks.
- Take it with food - one slice of toast, two crackers, or a small handful of nuts. No juice, no coffee, no water for 30 minutes after.
- Wait before moving - sit for 15 minutes after taking it. Don’t rush to shower or drive.
- Track it - write down the time you took it and how you felt. Did you feel nauseous? Dizzy? This helps your doctor adjust if needed.
- Use ginger - try 250 mg of ginger supplement 30 minutes before your dose if nausea is bad.
Patients who follow this plan have a 22% higher chance of sticking with the drug for six months, according to the manufacturer’s patient support program.
What to Do If It’s Not Working
If after 12 weeks you’re still nauseous, dizzy, or your blood sugar hasn’t improved, talk to your doctor. It might not be the right drug for you. There’s no shame in switching. Metformin, SGLT2 inhibitors, or GLP-1 agonists might be better fits - especially if your schedule is unpredictable or your nausea doesn’t improve.
But if you’ve given it time, stuck to the timing, and used the tips above, and your HbA1c dropped even a little while your heart health stayed stable - you’ve found something rare. A drug that doesn’t just treat sugar. It helps your whole body reset.

this drug sounds like a scam wrapped in a clinical trial
they got a 0.8% drop in HbA1c and called it a miracle
my cat could do better with a nap and a tuna sandwich
and don't get me started on the 'take it with toast' nonsense