For millions of people around the world, stomach pain, bloating, and erratic bowel habits aren’t just inconvenient-they’re life-limiting. Irritable Bowel Syndrome affects between 5% and 10% of the global population, yet most people still think of it as a simple digestive glitch. That’s outdated thinking. IBS isn’t just a gut problem. It’s a breakdown in the conversation between your gut and your brain. And understanding that connection is the key to real, lasting relief.
It’s Not Just Your Gut
For decades, doctors treated IBS like a malfunctioning pipe: too much gas, too little movement, or the wrong kind of stool. Treatments focused on calming the intestines with antispasmodics, laxatives, or anti-diarrheals. But for many, these didn’t work-or made things worse. The truth is, IBS isn’t caused by a broken colon. It’s caused by a broken signal. The gut and brain are wired together through what scientists now call the gut-brain axis. This isn’t just one pathway. It’s a whole network: nerves, hormones, immune cells, and even the trillions of microbes living in your intestines. When this system gets out of sync, your brain starts misreading signals from your gut. A normal amount of gas? Feels like cramping. A slight stretch in your bowel? Feels like sharp pain. That’s why people with IBS often feel pain where others feel nothing. Brain scans show clear differences in people with IBS. The part of the brain that handles emotions and pain-the prefrontal cortex-often shows reduced activity. Meanwhile, areas that process bodily sensations, like the insula and hypothalamus, become overactive. It’s like your brain’s volume knob for gut signals is turned up too high. And it’s not just in your head. Your gut lining changes too. Serotonin, the neurotransmitter that controls bowel movement and mood, is produced mostly in the gut. People with IBS-D (diarrhea-predominant) have up to 60% more serotonin in their intestinal lining than healthy people. Those with IBS-C (constipation-predominant) have too little. That’s why one person is always rushing to the bathroom and another can’t go for days-same diagnosis, opposite biology.Why Stress Makes Your IBS Worse
If you’ve ever felt your stomach knot up before a big presentation, you’ve felt the gut-brain axis in action. Stress doesn’t just make you anxious-it makes your gut scream. The HPA axis, your body’s main stress response system, directly influences gut motility, inflammation, and even the balance of your gut bacteria. In IBS, this system is hypersensitive. Even small stressors-like a tight schedule, a bad night’s sleep, or emotional tension-can trigger a flare-up. That’s why anxiety and depression are so common in IBS patients. Six in ten people with IBS also struggle with one or both. But it’s not that stress causes IBS. It’s that the same broken wiring that makes your gut hypersensitive also makes your brain more reactive to emotional stress. It’s a loop: gut pain → stress → worse gut pain → more stress. This is why simply taking a pill for pain or diarrhea often fails. You’re treating the symptom, not the signal. You need to reset the conversation.What Actually Works: Evidence-Based Relief
The good news? We now have treatments that target the gut-brain axis directly-not just the gut. Gut-directed hypnotherapy is one of the most powerful tools we have. It’s not about being put under a spell. It’s a structured form of guided relaxation that retrains your brain to interpret gut signals differently. In clinical trials, 70-80% of people who complete 6-12 sessions report major symptom improvement. And the benefits last. Unlike medication, the effects don’t vanish when you stop. It’s like reprogramming your brain’s alarm system. The low-FODMAP diet isn’t magic, but it’s science. FODMAPs are short-chain carbs that ferment in the gut, pulling water in and producing gas. For people with IBS, this triggers bloating, pain, and urgency. Cutting them out for 4-6 weeks helps 50-76% of people. But it’s not a lifelong diet. It’s a tool to identify triggers. Once you know which foods set off your symptoms, you can reintroduce others safely. Many people think they have to avoid broccoli, onions, and apples forever. They don’t. Most can tolerate small amounts after the elimination phase. Probiotics aren’t all the same. Not every yogurt or supplement will help. Only specific strains have been proven to work. Bifidobacterium infantis 35624, for example, has shown a 30-40% improvement in global IBS symptoms in multiple studies. That’s double the placebo effect. Other strains? Not so much. Look for products that list the exact strain and dose-1 billion CFUs or more. Medications are getting smarter too. Alosetron, a 5-HT3 blocker, works for severe IBS-D in women, reducing pain and diarrhea by half. Prucalopride, a 5-HT4 agonist, helps IBS-C by speeding up slow bowels. But these aren’t first-line options. They’re for when other treatments fail-and come with risks. Always talk to a specialist.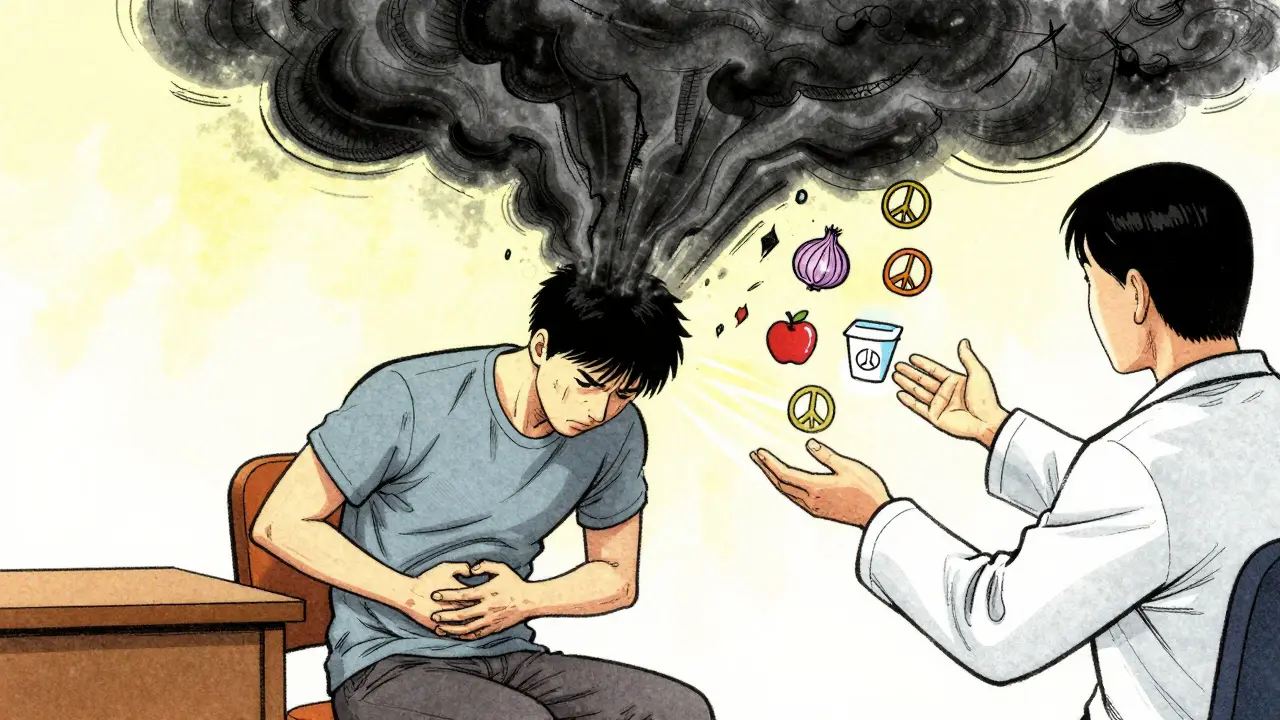
What Doesn’t Work (And Why)
Antispasmodics like dicyclomine or hyoscine might give you short-term relief, but they don’t fix the root issue. They just numb the muscle spasms. Many people stop taking them after a few weeks because they cause dry mouth, dizziness, or blurred vision-and the pain comes back. Loperamide (Imodium) slows diarrhea, but it doesn’t reduce pain or bloating. It masks the symptom while the brain-gut signal stays broken. And while some people swear by peppermint oil or fiber supplements, the evidence is mixed. Peppermint oil can help cramping for some, but it can also cause heartburn. Soluble fiber like psyllium helps constipation-predominant IBS, but insoluble fiber like wheat bran can make bloating worse for others. One size doesn’t fit all.Why Diagnosis Takes So Long
Most people with IBS wait 3-7 years to get diagnosed. Why? Because there’s no blood test, no scan, no biopsy that confirms it. Doctors have to rule out everything else first: celiac disease, Crohn’s, colon cancer, thyroid problems. That takes time-and visits. The Rome IV criteria are the gold standard: recurrent abdominal pain at least one day a week for three months, linked to bowel movements or changes in stool frequency or form. But many doctors still miss it. Especially if the patient doesn’t fit the “classic” profile. Women, older adults, and people with mostly bloating or discomfort (not pain) are often misdiagnosed. Understanding the gut-brain axis changes everything. When patients learn that their pain is real, but not caused by damage-it’s caused by miscommunication-they feel less blamed. A 2022 survey found that people who understood the brain-gut connection were 30% more likely to stick with treatment and 25% more likely to see improvement.
Where the Future Is Headed
The next wave of IBS treatment is personalization. Researchers are developing biomarker panels that measure microbial metabolites and neurotransmitter levels in the blood or stool. One test, called VisceralSense™, can predict with 85% accuracy which treatment will work for you-whether it’s hypnotherapy, a specific probiotic, or a new drug. Clinical trials are underway for drugs that target gut-brain pathways more precisely, like etrasimod, which showed over 50% symptom improvement in IBS-D patients. And the NIH just launched a $15 million project to map individual gut-brain profiles and build custom treatment plans. But access is still a problem. Gut-directed hypnotherapy requires a certified therapist. There’s only about one for every 500,000 people in rural areas. And insurance rarely covers it. The cost? $1,200-$2,500 out of pocket. That’s a barrier for many.Your Next Steps
If you have IBS, here’s what to do next:- Learn the gut-brain connection. Read up. Watch videos from reputable sources like the Mayo Clinic or the Rome Foundation. Knowledge reduces fear and increases control.
- Try a low-FODMAP diet with a dietitian. Don’t go it alone. A dietitian can help you eliminate, then reintroduce foods safely.
- Consider gut-directed hypnotherapy. Look for certified practitioners through the American Society of Clinical Hypnosis or similar bodies. Even 6 sessions can change your life.
- Choose the right probiotic. Look for Bifidobacterium infantis 35624 at 1 billion CFUs daily.
- Track your triggers. Use a simple app or journal to note food, stress, sleep, and symptoms. Patterns emerge over time.

This article is basically just a fancy ad for hypnotherapy and expensive probiotics. I’ve had IBS for 12 years and none of this crap worked. I just eat rice, chicken, and avoid everything. Done. No therapy needed. Stop selling me snake oil.