When you or someone you love starts a chemotherapy regimen that includes Capecitabine is an oral pro‑drug that the body converts into the active chemotherapy agent 5‑fluorouracil (5‑FU). While it’s effective against colorectal, breast, and gastric cancers, it also brings a set of oral side effects that can turn a simple toothpaste routine into a medical necessity.
Why dental health becomes a priority
Chemo drugs target fast‑growing cells, and the lining of your mouth is no exception. The result? Irritation, sores, dry mouth, and in rare cases, bone damage that can jeopardise a future dental implant. Ignoring these problems doesn’t just hurt - it can force a dose reduction or even a treatment pause.
Key oral complications linked to Capecitabine
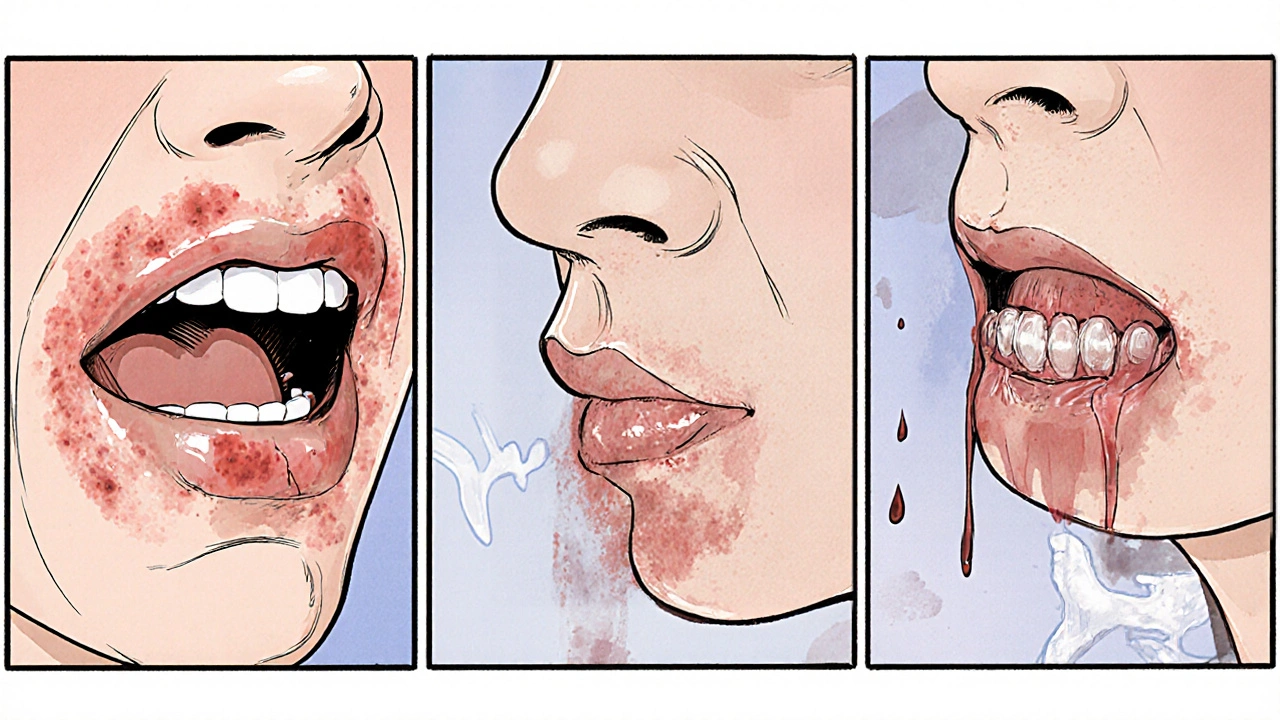
Understanding the most common mouth‑related issues helps you confront them early. Below is a quick snapshot.
| Condition | Typical onset | Primary symptom | First‑line management |
|---|---|---|---|
| Oral mucositis | 1-3 weeks | Painful ulcers | Gentle mouthwash, pain control, nutritional support |
| Xerostomia (dry mouth) | 2-4 weeks | Reduced saliva, sticky feeling | Saliva substitutes, frequent sips, fluoride rinse |
| Periodontal inflammation | 3-6 weeks | Bleeding gums, swelling | Professional cleaning, antimicrobial rinse |
| Osteonecrosis of the jaw (ONJ) | 6+ weeks (rare) | Expose bone, pain, infection | Stop invasive dental work, consult oral surgeon |
What is oral mucositis?
Oral mucositis is an inflammation of the mucous membranes lining the mouth, producing painful ulcerations that can make eating and speaking a challenge. It’s the most frequent complaint for patients on Capecitabine, affecting up to 40 % of users in clinical trials.
- Stay hydrated - sip water every 30 minutes.
- Use a bland, alcohol‑free mouthwash (e.g., saline or sodium bicarbonate solution).
- Ask your oncologist about low‑dose oral analgesics or topical lidocaine.
Managing xerostomia (dry mouth)
Xerostomia occurs when Saliva production drops, leaving the mouth dry, sticky, and more prone to decay. Capecitabine interferes with the autonomic nerves that stimulate salivary glands.
- Chew sugar‑free gum or suck on glycerin‑based lozenges to stimulate residual flow.
- Apply a fluoride‑rich toothpaste (1 % sodium fluoride) twice daily; ask your dentist for a prescription‑strength version if you’re at high risk.
- Avoid caffeine, alcohol, and tobacco - they worsen dryness.
Periodontal health: keeping the gums in check
Periodontal disease is inflammation of the supporting structures of the teeth, leading to bleeding, recession, and eventually bone loss. Reduced immunity from chemotherapy means bacteria can multiply unchecked.
Schedule a dental cleaning before you start Capecitabine and repeat it every 4-6 weeks while you’re on therapy. The dentist may prescribe a chlorhexidine rinse (0.12 %) for a short course to keep plaque at bay.
Osteonecrosis of the jaw (ONJ): the rare but serious risk
Although ONJ is more commonly linked to anti‑resorptive drugs (like bisphosphonates), case reports show it can appear under Capecitabine, especially when combined with radiation or steroids.
If you notice exposed bone that won’t heal for more than three weeks, contact an oral surgeon immediately. Preventive steps include:
- Never have extractions or implants during active chemotherapy.
- Maintain meticulous oral hygiene - the less bacterial load, the lower the infection risk.
- Discuss drug holidays with your oncologist if invasive dental work is unavoidable.
Preparing for treatment: a dental checklist
Before your first Capecitabine dose, run through this bite‑size list. It helps you avoid surprises and gives your oncology team confidence you’re ready.
- Book a comprehensive dental exam.
What to ask: “Do I have any active infections? Do I need extractions before chemo?” - Complete any needed cleanings, fillings, or root‑canal work.
- Get a professional fluoride varnish application.
- Discuss a personalized mouth‑care plan with the dentist - include prescribed rinses and fluoride toothpaste.
- Obtain a copy of your dental records and share them with your oncologist.
Daily oral‑care routine during Capecitabine
Adopt this hassle‑free schedule; it fits into a regular morning‑evening routine.
- Morning: Brush with a soft‑bristled brush and 1 % sodium fluoride toothpaste for two minutes. Rinse with a sugar‑free, alcohol‑free mouthwash.
- Mid‑day: Sip water, chew sugar‑free gum, or use a saliva substitute spray if dry.
- Evening: Repeat brushing, then finish with a fluoride rinse (no more than 30 seconds).
Replace your toothbrush every 2-3 weeks - the bristles wear out faster when you’re brushing gently but often.
When to call the dentist or oncology team
Not every sore needs a doctor, but some signs signal trouble.
| Symptom | Action |
|---|---|
| Persistent ulcer > 7 days | Phone dentist - may need a topical steroid. |
| Severe pain (VAS > 6) | Contact oncologist - adjust pain meds. |
| Bleeding gums that don’t stop | Schedule emergency cleaning. |
| Exposed bone or non‑healing socket | Urgent oral‑surgery referral. |
Nutrition tips that protect your mouth
What you eat can either soothe or inflame. Aim for soft, non‑acidic foods that require little chewing.
- Mashed potatoes, oatmeal, scrambled eggs.
- Cool soups (avoid very hot or spicy broths).
- Yogurt with probiotic cultures - supports oral microbiome.
- Avoid citrus, carbonated drinks, and rough granola.
Stay hydrated - at least 2 L of water daily. Dehydration worsens both xerostomia and mucositis.
Long‑term follow‑up after finishing Capecitabine
Even weeks after the last dose, your mouth may still be healing. Keep up the dental schedule for at least three months post‑treatment.
If you notice late‑onset problems like lingering dry mouth or new gum recession, bring them up at your survivorship clinic. Early intervention can prevent permanent damage.
Can I keep using my regular toothpaste while on Capecitabine?
Yes, but choose a fluoride‑rich, non‑abrasive formula. If you develop ulcerations, switch to a milder, alcohol‑free toothpaste until the sores heal.
Is it safe to get a dental cleaning during chemotherapy?
A professional cleaning is not only safe but recommended, provided your blood counts are within acceptable limits. Your oncologist can verify the timing.
What should I do if I develop a mouth ulcer that won’t heal?
Contact your dentist right away. They may prescribe a medicated mouthwash, a protective coating, or a short course of oral steroids to speed healing.
Does Capecitabine increase the risk of jaw bone loss?
The risk of osteonecrosis of the jaw is low but documented, especially when Capecitabine is combined with radiation or steroids. Preventive dental care cuts the odds dramatically.
Can mouth rinses with alcohol be used?
Avoid alcohol‑based rinses-they can further dry the mucosa and aggravate ulcers. Opt for chlorhexidine or saline solutions instead.
How often should I see my dentist while on Capecitabine?
Aim for a check‑up before treatment, then every 3-4 weeks during active therapy, and a final visit 6-8 weeks after the last dose.
Is there a link between Capecitabine and increased cavity risk?
Dry mouth reduces the natural cleansing action of saliva, which can raise cavity risk. Using fluoride toothpaste and regular rinses helps counteract this effect.

What they dont tell you is that capecitabine is just another tool in the elite's agenda, definatly part of a larger plan to keep populations dependent on pharma. The sideeffects are engineered to weaken the immune system and force regular dental visits under controlled conditions. This isnt a coincidence, it fits a pseudo‑philosophical narrative of power over the body. Stay vigilant and question every prescription.