When an alert flashes on your screen-whether it’s a security warning, a drug safety notice, or a system failure-your body doesn’t wait for you to think. Your heart jumps. Your breath tightens. Your mind races through worst-case scenarios. This isn’t weakness. It’s biology. And it’s happening to millions of people every day, especially in healthcare, IT, and emergency response roles. The good news? You can train your brain to respond differently. Not with willpower alone, but with proven, science-backed tools that work even when you’re overwhelmed.
Why Alerts Trigger Panic (And Why It’s Not Your Fault)
Your brain treats unexpected alerts like a tiger stepping into your living room. The amygdala, the part responsible for fear, kicks into overdrive. It shuts down the prefrontal cortex-the area you need to think clearly, weigh options, and make smart calls. Studies show this reduces decision-making ability by up to 67% during panic. Your heart rate spikes to 110-130 beats per minute. Breathing becomes shallow and fast. You fixate on one idea-maybe evacuate, maybe shut everything down, maybe call someone-while ignoring other critical details. This isn’t about being unprepared. It’s about how your nervous system evolved. Back then, a sudden noise meant danger. Now, it might mean a false alarm, a software glitch, or a routine safety update. But your body doesn’t know the difference. That’s why training your brain to pause before reacting isn’t optional-it’s essential.The First Step: Stop, Breathe, Ground Yourself
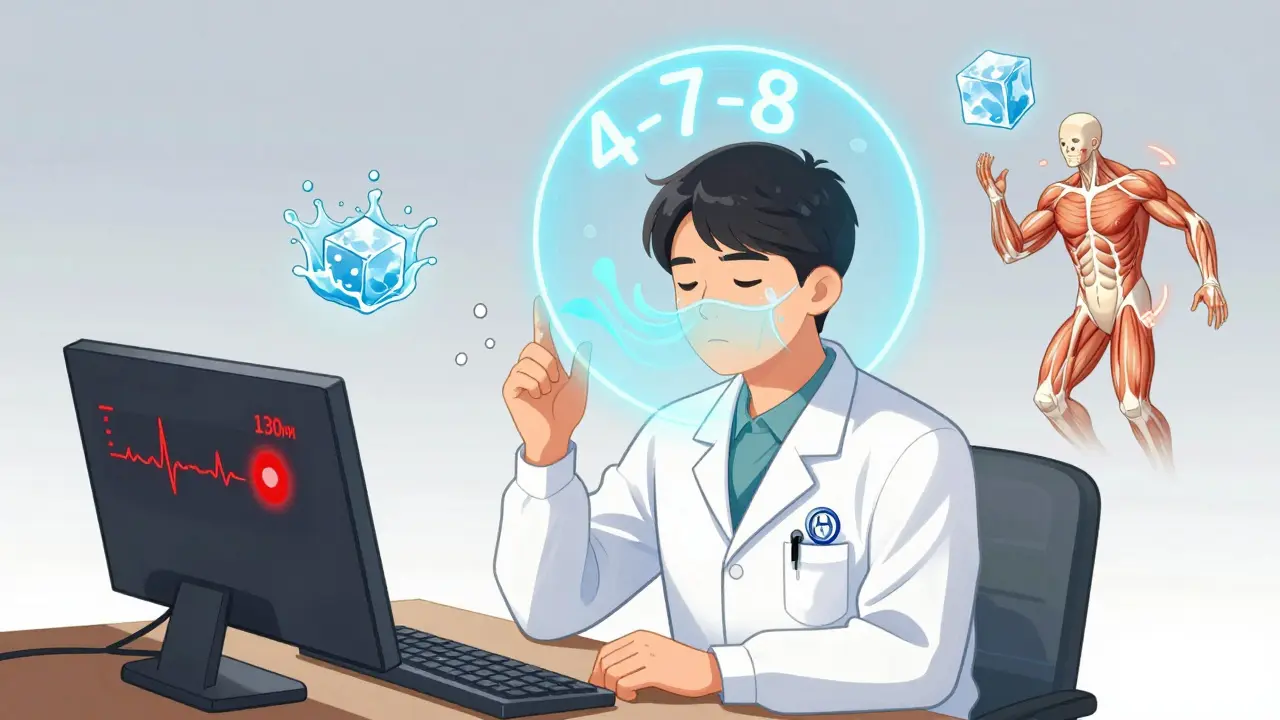
The quickest way to reset your nervous system isn’t to think harder. It’s to physically calm your body. Within 90 seconds, you can lower your heart rate from panic levels to a calm range (70-85 bpm) using controlled breathing. Try the 4-7-8 method: inhale for 4 seconds, hold for 7, exhale slowly for 8. Repeat three times. It sounds simple. But when your mind is screaming, this rhythm gives your brain something concrete to focus on. If breathing feels too hard in the moment, use the TIPP technique:- Temperature: Splash cold water (10-15°C) on your face. Or hold an ice cube in your hand for 20 seconds. Cold triggers the dive reflex, which slows your heart rate.
- Intense exercise: Do 30 seconds of jumping jacks or run in place. This burns off adrenaline.
- Paced breathing: Use the 4-7-8 method above.
- Paired muscle relaxation: Tense your fists for 5 seconds, then release. Move up to your arms, shoulders, jaw, and forehead. Release each group slowly.
Use the 5-4-3-2-1 Grounding Method to Reconnect with Reality
Panic pulls you into the future-imagining disasters that haven’t happened. Grounding pulls you back into the present. The 5-4-3-2-1 method works because it forces your brain to engage your senses, not your fears. Right now, look around and identify:- 5 things you can see (e.g., a coffee mug, a clock, a plant, your keyboard, a pen)
- 4 things you can touch (e.g., your shirt fabric, the desk surface, your watch, your shoes)
- 3 things you can hear (e.g., the hum of a fan, distant traffic, your own breath)
- 2 things you can smell (e.g., coffee, mint gum, fresh air from a window)
- 1 thing you can taste (e.g., toothpaste, a sip of water, a piece of gum)

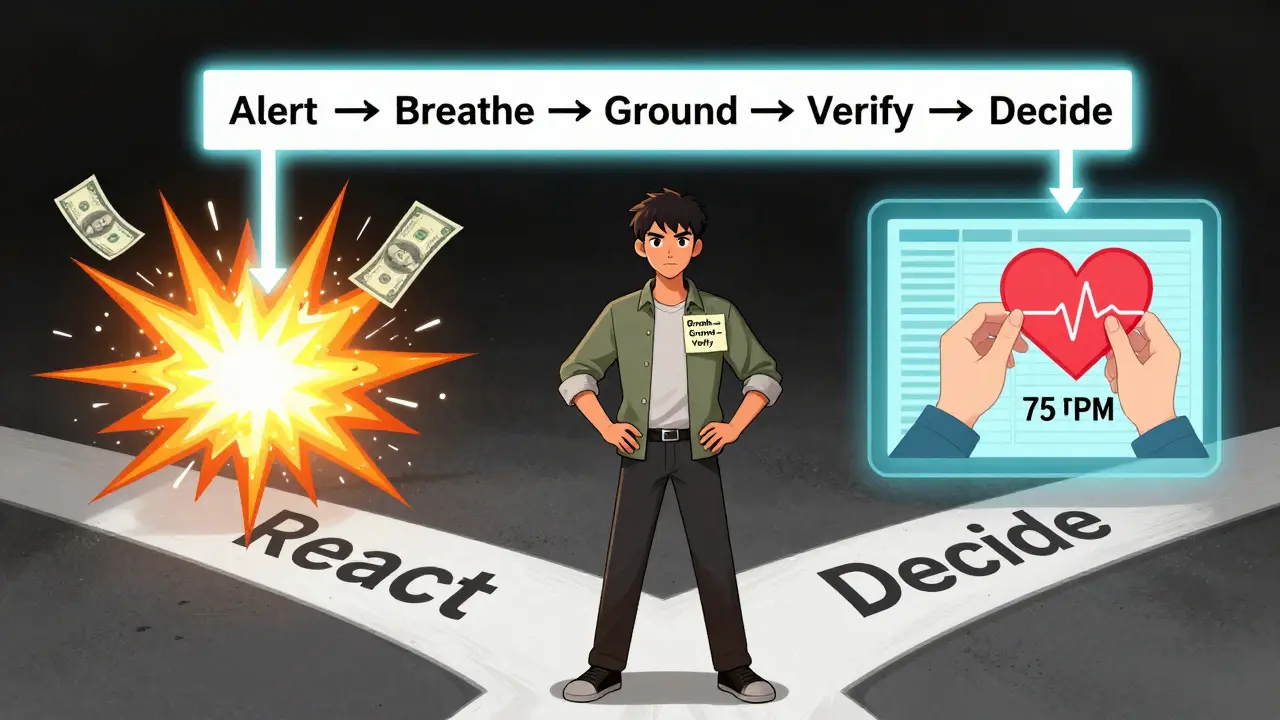
Make Decisions, Not Reactions: Use a Simple Decision Framework
Once you’re calmer, you need structure. Your brain is still under stress. It needs a map. The DEAR MAN technique helps you think clearly-even when you’re still feeling anxious.- Describe: State the alert factually. “The system flagged a potential drug interaction between X and Y.”
- Express: Say how you feel without blame. “I’m concerned this might be serious.”
- Assert: Ask for what you need. “Can I get the full patient history and lab results?”
- Reinforce: Explain why it matters. “If we act now, we prevent harm. If we wait, we risk delay.”
- Mindful: Stay focused on the facts. Don’t drift into “what ifs.”
- Appear confident: Even if you’re scared, speak calmly. Your tone influences others.
- Negotiate: “Is there another option? Can we monitor instead of act?”
Filter Decisions Through Your Core Values
When you’re stressed, it’s easy to act out of fear: “I have to fix this now.” But what’s your goal? Is it safety? Accuracy? Patient care? Avoiding liability? Ask yourself: “Does this action align with my core values?” If your value is “do no harm,” then rushing to cancel a drug order without checking the patient’s history might do more harm than good. If your value is “evidence-based action,” then you pause to verify data before acting. A 2022 study of 350 emergency responders found that those who used value-based filtering made 52% fewer regrettable decisions after alerts. You’re not just reacting-you’re choosing based on what matters.Prepare Before the Alert Happens
The biggest mistake people make? Waiting until the panic hits to learn what to do. By then, it’s too late. Your brain is flooded with cortisol. You won’t remember complex steps. Build a pre-alert routine:- Practice breathing or grounding for 10 minutes daily. Just 10 minutes a day for 8 weeks increases gray matter in your prefrontal cortex by 4.3%, improving your ability to stay calm under pressure.
- Get 7-9 hours of sleep. Poor sleep raises baseline anxiety by 31%.
- Limit caffeine to under 200mg a day (about two cups of coffee). More than that spikes cortisol and makes you more reactive.
- Move 150 minutes a week. Walking, cycling, yoga-any consistent movement lowers stress hormones.
- A smooth stone to hold (tactile grounding)
- A piece of mint gum (smell and taste trigger)
- A printed one-page reminder of your breathing technique and the 5-4-3-2-1 method
- A simple flowchart: “Alert → Breathe → Ground → Verify → Decide”
Technology Is Helping-But You Still Need to Be the Brain
New tools are emerging. Wearables now detect when your heart rate hits 100+ bpm and automatically trigger calming audio guides. AI systems are being built to guide users through step-by-step questions during alerts, reducing panic responses by over 50%. The EU’s DORA regulation now requires companies to include human stress response planning in their alert systems. But no app can replace your ability to pause, breathe, and choose. Technology supports. You lead.What Happens If You Don’t Do Anything?
The cost of unmanaged panic is real. In healthcare, rushed decisions lead to medication errors. In cybersecurity, false alarms trigger unnecessary shutdowns. In finance, panic selling causes financial loss. The average person now receives 67 alerts per week-up from 21 in 2018. Without tools to manage them, you’re not just stressed-you’re at risk of burnout, error, and regret. The good news? You don’t need to be perfect. You just need to be consistent. One person who practiced breathing daily for a month said, “I still get startled. But now I know how to come back. That’s everything.”Start Today. Not Tomorrow.
You don’t need a seminar, a certification, or a fancy app. You need one thing: practice. Tonight, before bed:- Take three slow 4-7-8 breaths.
- Identify five things you can see in your room.
- Write down one value that guides your decisions (e.g., safety, clarity, care).
What if I forget the techniques during a real alert?
Forgetting is common-especially if you’ve never practiced. The solution isn’t to memorize more. It’s to simplify. Pick one technique-like 4-7-8 breathing-and use it every day for 10 minutes. After 30 days, your body will auto-activate it during stress. Keep a printed reminder in your workspace. Even a sticky note with “Breathe → Ground → Verify” works.
Are these techniques only for healthcare workers?
No. Anyone who receives alerts-IT staff, financial traders, emergency responders, even parents managing school notifications-benefits. The science applies to any high-stress, high-stakes situation where quick, clear decisions matter. The alert might be a system warning, a market drop, or a child’s emergency call. The panic response is the same. So are the tools.
Can I use these techniques if I have a diagnosed anxiety disorder?
Yes. These are evidence-based tools used in CBT and DBT therapy, which are frontline treatments for anxiety disorders. Many people with anxiety diagnoses report improved control over panic responses after practicing these techniques regularly. But they’re not a replacement for professional care. If you’re struggling, work with a therapist to integrate these into your treatment plan.
How long does it take to see results?
You can feel calmer after one session. But lasting change takes consistency. Studies show that practicing for 10 minutes a day for 30 days makes techniques automatic. After that, you’ll notice faster recovery times, fewer impulsive decisions, and less lingering stress after alerts. The brain rewires itself with repetition-not intensity.
What if the alert is real and urgent? Should I still pause?
Yes-even in real emergencies. Panic leads to mistakes. A 10-second pause to breathe and ground yourself can prevent a costly error. For example, a nurse who paused to verify a drug alert instead of automatically canceling it found the patient had a documented allergy. That pause saved a life. Speed isn’t about rushing. It’s about acting correctly the first time.