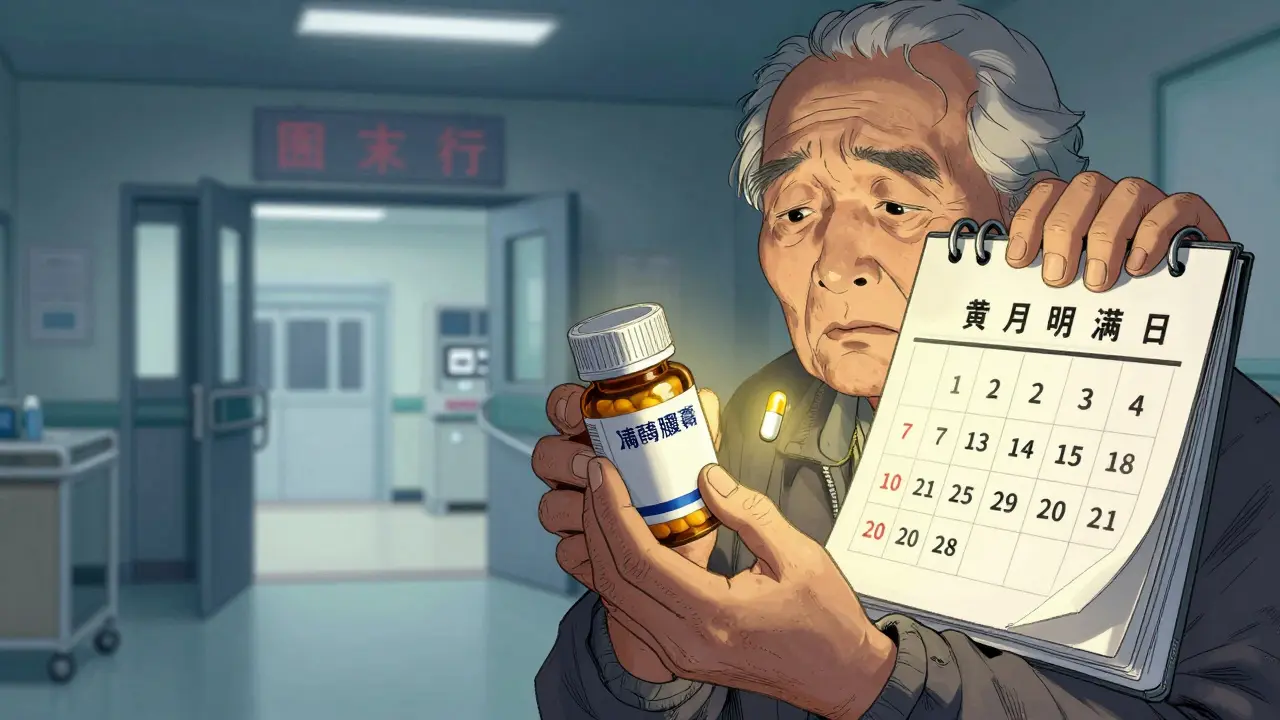
When a patient skips a dose because the pill costs too much, it’s not just a personal struggle-it’s a system failure. Medication adherence isn’t about forgetfulness. It’s often about affordability. And when generic drugs are priced right, adherence goes up, hospital visits go down, and lives get saved.
Why Cost Blocks Adherence
People don’t skip pills because they don’t care. They skip them because they can’t pay. A 2023 JAMA Network Open survey of over 2,100 adults found that 32.7% admitted to cutting doses, delaying refills, or skipping medications entirely to save money. That’s more than one in three. For someone managing diabetes, high blood pressure, or depression, that’s not a minor lapse-it’s a health emergency waiting to happen. The numbers tell the story. Every $10 increase in out-of-pocket cost for a prescription leads to a 2-4% drop in adherence, according to a 2022 review in the Journal of Managed Care & Specialty Pharmacy. For GLP-1 drugs used in diabetes, each $10 rise cuts adherence likelihood by 3.7% and pushes emergency room visits up by 5.2%. These aren’t abstract trends. They’re real people showing up in ERs because they couldn’t afford their daily pill.Generics Aren’t Cheap Copies-They’re the Same Medicine
Generic drugs aren’t second-rate. They’re exact copies. The FDA requires them to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they’re absorbed into the body at the same rate and to the same extent-within 80-125% of the brand. That’s not a guess. That’s science. And the price difference? It’s staggering. Generics cost 80-85% less than their brand-name counterparts. A brand-name statin like Crestor might cost $75 per month with a copay. The generic version, rosuvastatin,? $5. One patient on Reddit shared: “After my cardiologist switched me from brand-name Crestor to generic rosuvastatin, I went from missing 3-4 doses a week to perfect adherence for 11 months straight.” That’s not luck. That’s economics.When Price Drops, Adherence Rises
Real-world data confirms what theory predicts. In 2012, researchers studied Medicare Part D beneficiaries whose brand-name statins were moved from a higher-cost tier to a lower one. The result? A 5.9% increase in adherence measured by proportion of days covered. That’s not a small bump-it’s a major shift in behavior driven purely by price. Another study looked at women taking aromatase inhibitors after breast cancer treatment. Those on brand-name drugs had a 22.3% discontinuation rate. Those on generics? 17.8%. Adherence rates jumped from 68.4% to 73.1%. That’s a 4.7-point swing in compliance-just because the price dropped. And it’s not just heart or cancer meds. The same pattern shows up in mental health, asthma, and HIV treatment. When cost barriers come down, people take their meds. When they stay on their meds, they stay out of the hospital.The Hidden Cost of Non-Adherence
Skipping pills doesn’t save money-it costs more. Medication non-adherence leads to 50% of treatment failures. It contributes to over 100,000 preventable deaths every year in the U.S. And the financial toll? Between $100 billion and $300 billion in avoidable healthcare spending annually. Think about it: a $5 generic pill prevents a $15,000 hospital stay. A $10 copay stops a $50,000 ER visit. Studies show that patients who stick to their meds have 15-20% fewer hospitalizations. That’s not just better health-it’s better economics. The system is designed to ignore this. Insurance tiers, complex formularies, and surprise bills make it harder for patients to know what they’ll pay. That’s why real-time benefit tools (RTBTs) are changing the game. These tools show prescribers the exact cost of a drug before they write the script. In pilot programs, they’ve boosted adherence by 12-15%. One program reported a 40% reduction in care gaps and a 2:1 return on investment.
How the System Is Fixing Itself
Change is happening. The Inflation Reduction Act of 2022 capped insulin at $35 per month. By 2025, Medicare Part D will cap out-of-pocket drug spending at $2,000 a year. That’s huge for seniors on multiple medications. The FDA’s Generic Drug User Fee Amendments (GDUFA III), launched in 2023, are investing $1.1 billion to speed up generic approvals. By 2027, over 1,500 new generics could hit the market. That means more choices, more competition, and lower prices. Even better? Programs like Magellan’s inforMED use AI to predict who’s at risk of skipping meds because of cost-and reach out before they stop taking them. That’s proactive care. That’s smart economics.What Still Doesn’t Work
Despite the evidence, confusion lingers. Some patients still think generics are weaker. That’s a myth. The FDA’s “It’s Okay to Use Generics” campaign exists because people still believe it. Also, insurance formularies are a mess. A drug might be generic but still be in a high tier because of pharmacy benefit manager deals. That’s why tools like GoodRx help patients compare prices across pharmacies. Sometimes, the cash price at Walmart is lower than the insurance copay. Therapeutic duplication is another problem. Doctors sometimes prescribe two drugs for the same condition-like two different statins or two antidepressants. That’s 20-30% of avoidable spending. Medication therapy management programs can fix that by reviewing what a patient is actually taking.The Bigger Picture
Americans pay 256% more for brand-name drugs than people in other wealthy countries like Canada, Germany, or Australia. Yet, we still get the same pills. The difference? Our system lets drug companies set prices without limits. Generics break that cycle. In 2023, 90% of all prescriptions filled in the U.S. were generics. But they made up only 23% of total drug spending. That’s $643 billion saved between 2009 and 2019-just from using generics instead of brands. This isn’t about charity. It’s about efficiency. Lower prices lead to better adherence. Better adherence leads to fewer complications. Fewer complications mean lower overall costs. It’s a cycle that works.
What Patients Can Do
If you’re struggling to afford your meds:- Ask your doctor: “Is there a generic version?”
- Ask your pharmacist: “What’s the cash price?” Sometimes it’s cheaper than your copay.
- Use GoodRx or SingleCare to compare prices across local pharmacies.
- Ask about patient assistance programs-many drugmakers offer them for generics too.
- Request a real-time benefit check at your next appointment. If your doctor doesn’t use one, ask why.
so you're saying people are poor so they don't take pills? shocking. next you'll tell me water is wet.